We’re in an era experiencing a tectonic shift in foundations of medical imaging – MedCity News
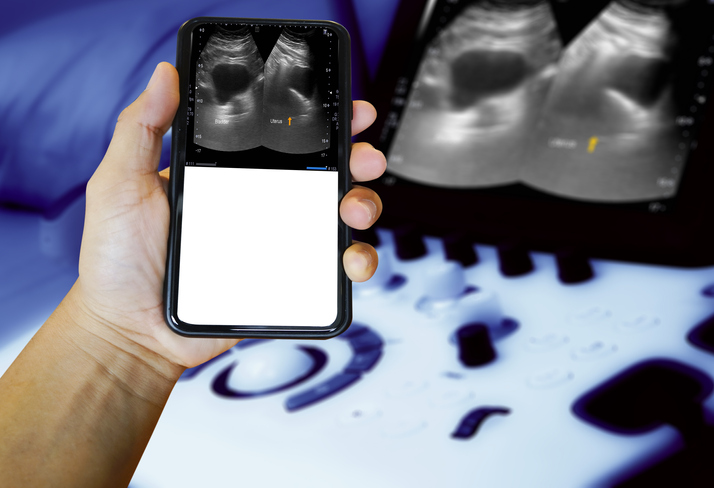
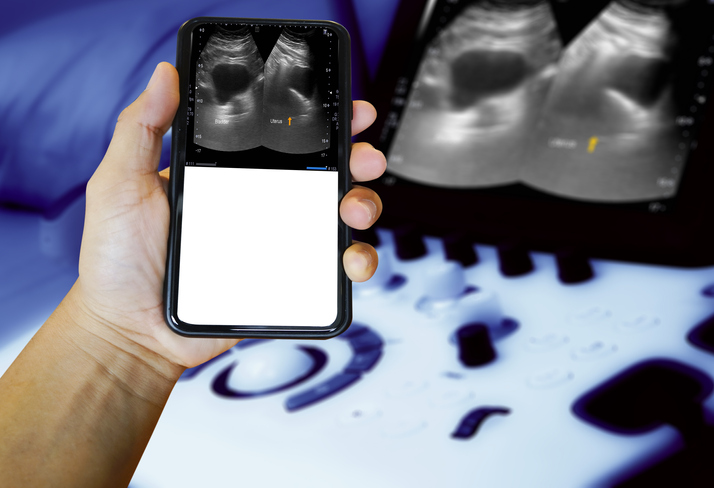
The future of diagnostic imaging is brighter than ever, even amid a perfect storm of challenges. An evolved state of point-of-care diagnosis and assessment is already being achieved in a large number of sectors across the industry. It’s happening through the use of next generation ultrasound, where imaging at-the-bedside vs. ordered from-the-bedside becomes possible and practical. It happens not because a cart was found and pushed into the room or because a referral was ordered. It happens because probe-based, handheld ultrasound now exists for all clinicians to create a window into the human body and in real-time to surface clinical insights to power better clinical decisions.
“The future is already here, it’s just not very evenly distributed,” a famous author once wrote. That’s pretty much the case in today’s portable ultrasound world. While thousands of clinicians have adopted pocket-based, point-of-care ultrasound to enhance how they diagnose and treat patients, not all have. If embraced more fully and thoughtfully, this new way of diagnostics will establish a new standard of care and revolutionize what’s possible between clinicians and their patients. Here’s a look at three major trends driving today’s rapid move towards the adoption of portable ultrasound.
Growing Demand for Economic Efficiency
Today’s healthcare industry is facing intense pressures. Of particular concern to ultrasound professionals is greater demand for imaging procedures coupled with post-Covid clinician exhaustion and burnout. At the same time, many hospitals and healthcare enterprises are facing intense cash flow problems and demanding greater efficiency. As the baby boom population ages, utilization rates of diagnostic imaging have risen rapidly relative to other health services in the United States. On top of all this, the number of those entering the healthcare workforce in many specialties continues to dwindle. Some states already have nearly 30% fewer providers compared to patients who demand imaging services.
Today’s handheld imaging equipment can be used in many clinical settings where ultrasound has not traditionally been utilized or found. This allows more practitioners to gain access to valuable clinical insights and deliver better, more effective care.
Paramedics, for example, have effectively introduced handheld ultrasound into cardiac assessment without disrupting resuscitation protocol. Other care teams are using handheld ultrasound to determine heart failure without the need to order and await the results of a chest X-ray. By rethinking old rules constraining where, how and who could use diagnostic imaging effectively—and leveraging AI to provide robust diagnosis guidance that accelerates physicians’ journey to competency—healthcare professionals today are overcoming the limits of too few machines and too few traditionally trained professionals.
Limited Access to Care
It’s not just growing demand that is taxing the system, it’s also the many prospective patients out there who have poor geographical access to it. Too often, patients exhibiting any number of symptoms are sent by their local physicians to larger hospital facilities for medical imaging tests to establish or confirm diagnoses. For patients in most parts of the U.S. who don’t live in large cities, that exacts a steep cost in time and travel, and so often, they neglect getting care or delay it so significantly that their medical issues worsen before the diagnosis is final. And the challenges of those in the rural U.S. is just the tip of the iceberg: A full two-thirds of the world—4.7 billion people—lack access to medical imaging altogether.
Possible from a small, stapler-sized probe that links to smartphones for display, the wonder of advanced ultrasound is it largely makes these problems of geographic limits obsolete. Practitioners everywhere can have ready-to-use assessment tools in their pockets.
Protracted Training. Vast medical databases, accessible via the cloud and capable of being analyzed by powerful AI algorithms, provide physicians today with robust guidance to help build accurate diagnoses. Evolved handheld ultrasound provides physicians with some of today’s most advanced point-of-care tools, semiconductor-based and AI-enabled, that do not require years-long intensive training and are unencumbered by the cart and referral model altogether.
Capturing and interpreting ultrasound is today eased and simplified. The top levels of government recognize the import of this change. The Center for Medicare and Medicaid Services (CMS) has a designation, NTAP, awarded to new medical technologies that are expected to substantially improve the diagnosis or treatment of Medicare beneficiaries. Such designation has been recently granted to an AI-guided ultrasound software as well. Medical schools are providing imaging probes for every medical student and incorporating training into their core curriculum. Some home health companies are arming their clinicians with probes for home-based care. Ambulances and helicopters include ultrasound probes as part of standard equipment. Even sports teams are bringing real-time imaging to the sidelines and training rooms to more quickly understand what’s happening inside an athlete’s body.
For decades, ultrasound machines and enterprise diagnostic imaging deployments have cost anywhere from tens to upwards of several hundred thousands of dollars. While newer POCUS technology will not replace high-end imaging assessments, it does provide a tectonic shift in the foundations of imaging as a practical diagnostics advisor at the bedside.
Photo: Tonpor Kasa, Getty Images