Update on Medicaid Coverage of Gender-Affirming Health Services
Transgender and nonbinary adults often face challenges and barriers to accessing needed health services and face worse health outcomes than their cisgender peers. Transgender adults are more likely than cisgender adults to be uninsured, report poor health, have lower household incomes, and face barriers to care due to cost. Given their lower incomes, Medicaid plays an important role in health coverage for transgender people. A 2019 report by the Williams Institute estimated that among the 1.4 million transgender adults living in the United States, approximately 152,000 had Medicaid coverage.
Medicaid is the country’s health coverage program for low-income people and is jointly funded by the federal government and states. Under Medicaid, states must cover certain mandatory benefits, such as inpatient and outpatient services, home health services, and family planning services. While there are no specific federal requirements regarding coverage or exclusion of gender-affirming health care services as a category of Medicaid benefits, there are rules regarding comparability requiring that services must be equal in amount, duration, and scope for all beneficiaries within an eligibility group.
Medicaid benefits are subject to Section 1557 of the Affordable Care Act (ACA), the law’s major non-discrimination provisions, which prohibit discrimination based on sex. The Biden Administration recently proposed a new rule on Section 1557 that explicitly states that it interprets, and will enforce, sex-based protections to include sexual orientation and gender identity. The administration had already asserted this position in guidance stating that under 1557 protections, “categorically refusing to provide treatment to an individual based on their gender identity is prohibited discrimination” and it returns to a position more closely aligned to that under the Obama administration but walked back under the Trump administration.
Despite these protections, some states have recently moved to implement or consider actions aimed at limiting access to gender-affirming health care, particularly for youth. This has included restrictions on coverage of benefits as well as bans on the provision of gender-affirming care by health care providers. A number of lawsuits are pending.
| Gender Identity: One’s deeply held, internal sense of self as masculine, feminine, a blend of both, neither, or something else. Identity also includes the name used to convey one’s gender. Gender identity can correspond to or differ from the sex assigned at birth. |
| Transgender: Somebody who is transgender has a gender identity different from that traditionally associated with sex assigned at birth. |
| Non-binary: An umbrella term for gender identities that are not exclusively masculine or feminine. |
| Cisgender: Refers to people whose gender identity aligns with their assigned sex at birth |
| Gender dysphoria: “A concept [and clinical diagnosis] designated in the DSM-5 as clinically significant distress or impairment related to a strong desire to be of another gender, which may include desire to change primary and/or secondary sex characteristics. Not all transgender or gender diverse people experience dysphoria.” |
| Gender-affirming care: Gender-affirming care is a model of care which includes a spectrum of “social, psychological, behavioral or medical (including hormonal treatment or surgery) interventions designed to support and affirm an individual’s gender identity.” |
| SOURCES: Gender Spectrum, The Language of Gender, Accessed October 3, 2022; American Psychiatric Association, What is Gender Dysphoria?, August 2022; OASH Office of Population Affairs, Gender-Affirming Care and Young People, Accessed October 3, 2022. |
What gender affirming services do states report covering through Medicaid?
The standards of care for gender-affirming health services set by the World Professional Association for Transgender Health include hormone therapy, surgeries, fertility assistance, voice and communication therapy, primary care, and behavioral health interventions. Additionally, the Endocrine Society supports gender-affirming care in their clinical practice guidelines. Together, these guidelines form the standard of care for treatment of gender dysphoria. Gender-affirming care is highly individualized, and while not all transgender and nonbinary individuals will want or seek any or all of these medically necessary services, limiting access to them can lead to negative and life threating outcomes. Major U.S. medical associations, such as the American Medical Association, the American College of Obstetricians and Gynecologists, the American Academy of Nursing, the American Psychiatric Association, among others, have issued statements underscoring the medical necessity of gender-affirming care.
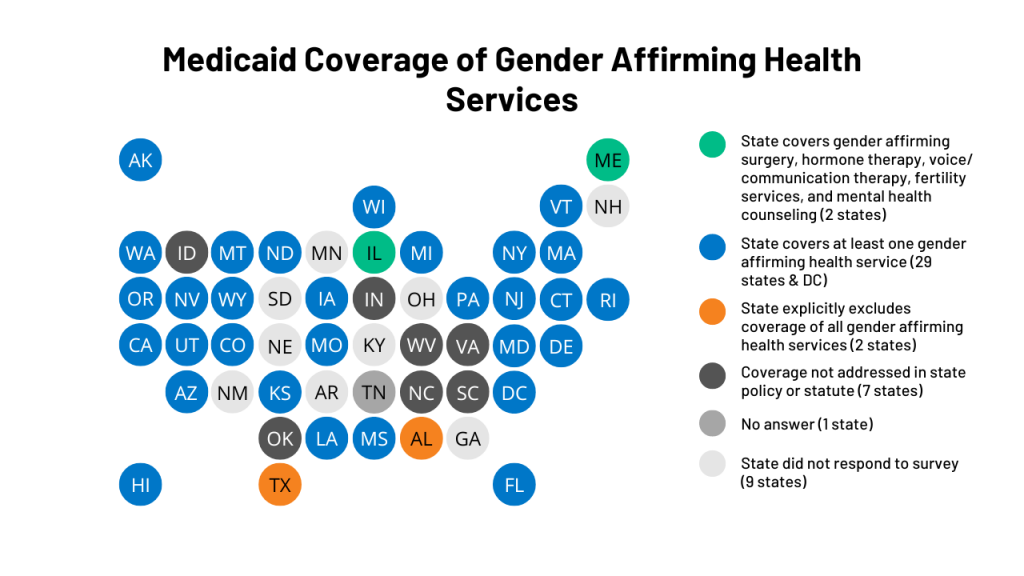
In a survey of states on coverage of sexual and reproductive health services conducted in Summer 2021, KFF and Health Management Associates (HMA) asked states about coverage of five gender-affirming care services: gender-affirming counseling, hormones, surgery, voice and communication therapy, and fertility assistance for transgender enrollees (Questions presented in Appendix Table 1). Because the survey focused on adult access, states were not asked about puberty blocking hormones. States were asked if a service was covered, excluded from coverage, or whether coverage was not addressed in state policy or statute for adults over the age of 21, as of July 1, 2021. Services that are not addressed in state policy or statute may or may not be covered by the state, or coverage may vary by case. The survey instrument was distributed via email to state Medicaid directors and where applicable, Medicaid agency staff working on women’s health and reproductive health issues. Forty-one states and the District of Columbia responded to the survey. Tennessee responded to the survey but did not answer questions related to gender-affirming services. Survey findings are summarized in Figure 1 and Table 1 and highlights are presented below.
Overall coverage of gender-affirming care:
As detailed below, many state Medicaid programs cover aspects of gender-affirming health services. However, only two of the 41 states responding to this survey, Maine and Illinois, reported covering all five services. Two states, Alabama and Texas, reported they do not cover any of these services under Medicaid.
Gender-Affirming Hormone Therapy:
Gender-affirming hormone drugs include estrogen, anti-androgens, and progestins (feminizing hormones), as well as testosterone and other agents (masculinizing hormones). Under federal law, and subject to exceptions for a few drugs or drug classes, state Medicaid programs are required to cover all drugs from manufacturers that have entered into a rebate agreement with the Secretary of Health and Human services under the federal Medicaid Drug Rebate program. Twenty-five states reported covering gender-affirming hormones, and 10 of these states require prior authorization. Thirteen states said coverage was not addressed in state statute or policy, and three states—Alabama, Hawaii, and Texas —exclude coverage of gender-affirming hormone therapy.
Gender Affirming Surgery:
Gender-affirming surgery can include chest surgery, genital surgery, facial surgery, and other surgical procedures aimed at helping a transgender or nonbinary person transition to their self-identified gender. Not all transgender or nonbinary individuals seek or want surgical treatments. Twenty-three of the 41 responding states reported covering gender-affirming surgery for adults through their state Medicaid programs. Nine states reported coverage was not addressed in state statute or policy, and nine states reported that they excluded gender-affirming surgery from coverage. This survey did not ask states to specify what surgical procedures they cover, but some states provided additional details, which can be found in Appendix Table 2.
Ten of 23 covering states require prior authorization. For example, Colorado requires a clinical diagnosis of gender dysphoria and that the patient has lived in their preferred gender for 12 continuous months. Colorado and Wisconsin also require that the patient has completed 12 continuous months of hormone therapy.
Voice and Communication Therapy
Some transgender people have challenges with developing a voice that matches their gender identity. Voice therapy services can encompass a range of treatments that address pitch, intonation, articulation, pragmatic speech and other aspects of communication.
Thirteen of the 41 responding survey states report that they cover gender-affirming speech or voice therapy services, some requiring prior authorization. Ten of the survey states reported that they exclude coverage for gender-affirming voice therapy services, and 18 states responded that they have not addressed this coverage in their state policy.
Fertility Services:
A broad array of diagnostic and treatment services are available to assist with achieving a pregnancy. Diagnostics typically include lab tests, semen analysis and imaging studies, or procedures of the reproductive organs. Treatment services include medications, reproductive system procedures to allow for pregnancy, and an array of other interventions to help an individual achieve pregnancy, such as intrauterine insemination (IUI) and in-vitro fertilization (IVF). While federal rules require states to cover most prescription medications under Medicaid, there is an exception that allows states to exclude coverage for fertility medications.
Fertility services can be unaffordable without insurance coverage but few states (11) cover services for any beneficiaries, regardless of gender identity. In this survey, just three states (Illinois, Maryland, and Maine) reported covering fertility services as part of gender-affirming care. Of these three states, Illinois is the only one that reported covering services for beneficiaries without exceptions. More than half of states (29) reported that they exclude coverage for fertility services for transgender individuals, and nine states responded that they have not addressed this coverage in their state policy (Table 1).
Mental Health Counseling:
Transgender and nonbinary individuals may seek mental health services to address issues related to their gender identity and transition but may also seek care to address issues that are not related to their gender transitions. As noted, in some cases a diagnosis of gender dysphoria is required before gender-affirming services can be accessed.
Twenty-seven states reported covering mental health counseling and services specifically related to gender affirming health services, 11 states reported coverage was not addressed in their state statute or policy, and three states, Alabama, Kansas, and Texas, reported that they exclude this benefit.
Some states reported requiring that transgender and non-binary Medicaid enrollees receive mental health assessments prior to receiving hormone therapy or having gender-affirming surgeries. For example, Delaware requires prior authorization for mental health counseling related to gender-affirming care, and Connecticut reported that depending on the type of service, prior authorization may be required.
Conclusion
The need for coverage of and access to medically necessary gender-affirming care has been recognized by leading medical and health professional organizations. However, some states have enacted laws banning the provision of gender-affirming health services to youth, and coverage for gender-affirming health services is uneven in state Medicaid programs. In most states, there is variation in coverage for specific services and some states do not have policies addressing coverage in their state Medicaid programs, potentially leaving many low-income transgender and nonbinary individuals without access to medically necessary health services.
Since this survey was conducted, the Biden Administration has proposed a new rule on Section 1557, which is consistent with their prior guidance, and proposes that excluding coverage for gender-affirming care constitutes sex discrimination. In addition, beyond what is stated in rulemaking by the current or previous administrations, some courts have found that the statue itself (i.e., sex non-discrimination provisions) protects against health care discrimination based on gender identity and sexual orientation. For example, a federal district court permanently enjoined the Wisconsin Medicaid program from categorically excluding gender-affirming services from coverage, relying on the statute. Similarly, in recent months, federal courts have ruled the Georgia and West Virginia must cover gender-affirming care in their Medicaid programs. Most recently, in June 2022, Florida’s Medicaid agency announced it would ban coverage of gender-affirming health services in the state. The policy went into effect in August and was challenged in court a few weeks later (with the case still pending). States that do not cover components of gender-affirming care may be in violation of Sec. 1557 of the ACA. However, there are a number of pending legal challenges to the Sec. 1557 rule as well as over specific Medicaid state policies related to coverage of gender-affirming services which will be important to watch moving forward to fully understand this evolving landscape.