| United States |
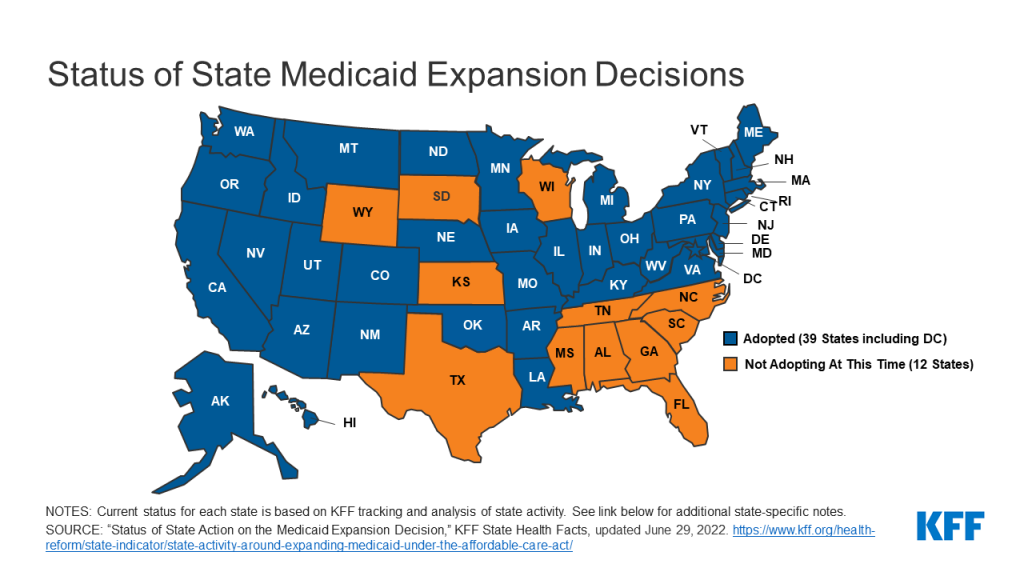
Coverage under the Medicaid expansion became effective January 1, 2014 in all states that have adopted the Medicaid expansion except for the following: Michigan (4/1/2014), New Hampshire (8/15/2014), Pennsylvania (1/1/2015), Indiana (2/1/2015), Alaska (9/1/2015), Montana (1/1/2016), Louisiana (7/1/2016), Virginia (1/1/2019), Maine (1/10/2019 with coverage retroactive to 7/2/2018), Idaho (1/1/2020), Utah (1/1/2020), Nebraska (10/1/2020), Oklahoma (7/1/2021), and Missouri (Processing applications beginning 10/1/2021 with coverage retroactive to 7/1/2021).
Arizona, Arkansas, Indiana, Iowa, Michigan, Montana, and Utah have approved Section 1115 waivers to operate their Medicaid expansion programs in ways not otherwise allowed under federal law. In some states, these included previously-approved Section 1115 work requirements that have since been withdrawn by CMS under the Biden Administration.
|
| Arkansas |
In December 2021, CMS approved Arkansas’ Section 1115 waiver request which would replace the state’s current Medicaid expansion program, Arkansas Works, with the Arkansas Health and Opportunity for Me (ARHOME) program. CMS also notified Arkansas that it would phase out the state’s premium requirement for the expansion population by the end of 2022. Unlike Arkansas Works, ARHOME does not include work requirements. Under ARHOME, Arkansas is requesting to allow the state’s Qualified Health Plans (QHPs) to incentivize enrollee participation in health and economic independence initiatives and to consider QHP enrollees who do not participate in these incentives as “inactive” and reassign them to the state’s fee-for-service program; this aspect of the request is still pending CMS approval. |
| Idaho |
Enrollment in Medicaid coverage under expansion began on November 1, 2019, and coverage for these enrollees began on January 1, 2020. Following a successful expansion ballot measure in November 2018, in 2019 Governor Brad Little signed a bill passed by the legislature that directed the Idaho Department of Health and Welfare to seek waivers for multiple changes to the expansion program and specified that if the waivers were not approved by January 1, 2020, then all individuals up to 138% FPL will be enrolled in Medicaid. The state submitted four waivers at direction from this legislation; however, only one has been approved to date. |
| Kentucky |
On December 16, 2019, newly elected Democratic Governor Andy Beshear signed an executive order rescinding the Kentucky HEALTH waiver that had been set aside by the court in March 2019. The waiver had included a number of provisions including a work requirement, monthly premiums up to 4% of income, and coverage lockouts for failure to timely renew eligibility or timely report a change in circumstances. Kentucky’s expansion program was originally implemented and continues to operate under state plan amendment (SPA) authority. |
| Maine |
Maine implemented expansion on January 10, 2019. Maine adopted the Medicaid expansion through a ballot initiative in November 2017. After former Governor LePage delayed implementation of the expansion for months, new Governor Mills signed an executive order on her first day in office (January 3, 2019) directing the Maine Department of Health and Human Services to begin expansion implementation and provide coverage to those eligible retroactive to July 2018. CMS approved the state’s plan retroactive to July 2, 2018 on April 3, 2019. |
| Missouri |
In February 2022 the Missouri House passed a bill proposing a legislatively referred constitutional amendment that would impose work requirements on expansion enrollees and would also subject Medicaid expansion to legislative appropriations each fiscal year; however, the 2022 legislative session adjourned without the bill’s passage in the Senate. Missouri voters originally approved a ballot measure in August 2020 that added Medicaid expansion to the state’s constitution and prohibited any additional burdens or restrictions on eligibility for the expansion population. Medicaid coverage under expansion began when the state started accepting applications in August 2021 and began processing applications in October 2021, with coverage retroactive to July 1, 2021 consistent with a state supreme court order.
Previously, Governor Mike Parson announced that the state would not implement expansion because the ballot measure did not include a revenue source. In May 2021, individuals who would be eligible for expansion coverage filed a lawsuit against the state. However, in July 2021, the Missouri Supreme Court ruled that the initiated amendment is valid under the state constitution and that the legislature’s budget appropriation authorizes the state to fund expansion coverage.
|
| Montana |
In December 2021, CMS notified Montana that it would phase out the state’s Section 1115 premium requirement for the expansion population by the end of 2022. Per May 2019 state legislation, Montana submitted a Section 1115 waiver amendment in August 2019 requesting to add a work requirement as a condition of eligibility and to increase the premiums required of many beneficiaries. CMS under the Biden Administration is unlikely to approve this pending request given the agency’s phase-out of Montana’s existing premium requirement and withdrawal of work requirement waiver provision in other states. |
| Nebraska |
Enrollment in Medicaid coverage under expansion in Nebraska began on August 1, 2020, and coverage for these enrollees began on October 1, 2020. Nebraska voters had approved a Medicaid expansion ballot measure in November 2018, and the state delayed implementation to allow time to seek a Section 1115 waiver to implement expansion with program elements that differ from what is allowed under federal law, including a tiered benefit structure that requires beneficiaries to meet work and healthy behavior requirements to access certain benefits. While CMS approved this waiver on October 20, 2020, on August 17, 2021, the state requested to withdraw its approved waiver, which CMS subsequently approved on September 2. The state announced that it plans to offer all expansion adults full benefits starting October 1, 2021. |
| Oklahoma |
Enrollment in Medicaid coverage under expansion in Oklahoma began on June 1, 2021, with coverage for these enrollees beginning on July 1, 2021. Oklahoma voters approved a ballot measure on June 30, 2020 which added Medicaid expansion to the state’s Constitution. Language in the approved measure prohibits the imposition of any additional burdens or restrictions on eligibility or enrollment for the expansion population. |
| Utah |
Medicaid coverage under expansion began on January 1, 2020. Following a successful Medicaid expansion ballot measure in November 2018, the state legislature took steps to roll back the full expansion by directing the state to submit a series of Section 1115 waivers. On December 23, 2019, CMS approved certain provisions in the state’s “Fallback Plan” waiver request to amend its Primary Care Network Waiver to expand Medicaid eligibility to 138% FPL, effective January 1, 2020; the approval also included work requirements for the newly expanded adult Medicaid population. In February 2021, the Biden Administration began to withdraw waivers with work requirement provisions |
| Virginia |
The Virginia General Assembly approved Medicaid expansion as part of its FY 2019-2020 budget on May 30, 2018; Governor Northam signed the budget into law on June 7, 2018. Expansion coverage became effective under state plan amendment (SPA) authority on January 1, 2019 after enrollment began on November 1, 2018. |
| Florida |
An initiative to put Medicaid expansion on the 2020 ballot was delayed by its organizing committee. |
| Georgia |
In December 2021, CMS under the Biden Administration withdrew Georgia’s Section 1115 approval for work and premium requirements in the state’s Pathways to Coverage waiver. However, in January 2022, Georgia filed a lawsuit in federal court challenging the CMS’ withdrawal. The waiver, which would not be a full Medicaid expansion under the ACA and would not qualify for enhanced matching funds, was initially approved in October 2020 and gave Georgia authority to extend Medicaid coverage to 100% FPL for parents and childless adults. Initial and continued enrollment would have been conditioned on compliance with the now-withdrawn work and premium requirements. The state is not implementing the coverage provisions while pursuing litigations |
| Kansas |
On January 12, 2022, Democratic Governor Laura Kelly included Medicaid expansion in her proposed budget for State Fiscal Year (SFY) 2023 that accounts for additional federal Medicaid matching funds due to the American Rescue Plan Act (ARPA) incentive for states to newly adopt expansion; separately, in February 2022 Kelly proposed expansion legislation that also includes a work referral program. However, the Republican-controlled legislature did not include expansion in its final SFY2023 budget, and the 2022 legislative session adjourned without additional action on Kelly’s proposed legislation. In 2021, Governor Kelly had previously included Medicaid expansion in her proposed budget for SFY 2022 (before the ARPA incentive was available) and proposed expansion legislation that included premiums and a work referral program and funded with revenue from medical marijuana sales; the 2021 legislative session adjourned with any additional action on the bill and the final SFY 2022 budget did not include expansion. A similar bill from 2020 had broad bipartisan support but was funded through a reinsurance program and hospital surcharge. That bill was blocked from progressing in the Senate over an anti-abortion debate. |
| Mississippi |
Although Mississippi’s Secretary of State approved a 2022 Medicaid expansion ballot initiative for circulation in April 2021, on May 19 the organizing committee suspended its campaign following a Mississippi Supreme Court decision ruling that the state’s entire ballot initiative process is inoperable due to procedural errors regarding ballot initiative language in the state’s constitution. While Medicaid expansion was a key issue in the 2019 Mississippi gubernatorial election, current Republican Governor Tate Reeves opposes expansion, making it unlikely that the state will take up expansion through legislation. |
| North Carolina |
On June 2, 2022, the North Carolina Senate passed a bill that would expand Medicaid. If enacted, the bill would implement the expanded coverage no later than July 1, 2023. Additionally, the bill directs the state to seek federal approval to impose work requirements on beneficiaries as a condition of eligibility on expansion enrollees. Although the bill has not advanced in the House, the House passed a separate bill on June 28, 2022 that would establish a joint legislative study committee tasked with voting on a recommended Medicaid expansion plan in December 2022. In addition, the House bill would direct the state to create a Medicaid work referral program and seek federal approval to condition Medicaid eligibility on compliance with work requirements, if CMS indicates that it may approve such work requirements.
Previously, Democratic Governor Roy Cooper proposed Medicaid expansion in his state budget proposals for both State Fiscal Years (SFY) 2020-2021 and 2022-2023;however, the Republican-controlled legislature did not include expansion in either final budget. In Governor Cooper signed the SFY 2022-2023 budget that again omitted expansion, although the budget bill did establish a legislative committee to study Medicaid expansion and potentially propose legislation. In 2019, Governor Cooper vetoed the SFY 2020-2021 budget due to omission of Medicaid expansion and the 2019 legislative session resulted in a budget impasse.
|
| South Carolina |
On December 12, 2019, CMS approved two separate 1115 waivers for South Carolina which would extend Medicaid coverage from 67% to 100% FPL for its parent/caretaker relative groups and a new targeted adult group with initial and continued enrollment conditioned on compliance with work requirements at the regular match rate; this coverage would not qualify as a full Medicaid expansion under the ACA. In February 2021, the Biden Administration began to withdraw waivers with work requirement provisions. |
| South Dakota |
In 2022, South Dakota’s Secretary of State validated two Medicaid expansion ballot initiatives for the November 2022 ballot, submitted by two separate ballot committees. One of the validated initiatives is a constitutional amendment that specifies that South Dakota must implement expansion coverage beginning July 1, 2023, while the other validated initiative is an initiated state statute. Both ballot measures include language prohibiting the imposition of any additional burdens or restrictions on eligibility and enrollment for the expansion population. If approved by voters, initiated state statutes in South Dakota can be repealed or amended by the state legislature; however, the legislature cannot make changes to an initiated constitutional amendment without legislatively referring a subsequent ballot measure to voters.
A legislatively referred constitutional amendment validated for the June 2022 ballot would have directly challenge the Medicaid expansion ballot initiatives by increasing the voter approval threshold from 50% to 60% for any petitions that would require more than $10 million in state appropriations; however, it was defeated by voters.
|
| Wisconsin |
After the Wisconsin Legislature’s Joint Finance Committee voted to remove Medicaid expansion funding from Democratic Governor Tony Evers’ State Fiscal Years (SFY) 2022-2023 budget proposal, Governor Evers signed an executive order to hold a special session for Medicaid expansion legislation on May 25, 2021, proposing to use the additional federal funds the state could receive under the incentive in the American Rescue Plan Act for other state development projects. However, on May 25, the Republican-controlled legislature adjourned the special session without further action, and the legislature passed a SFY 2022-2023 budget without Medicaid expansion funding on June 30. The governor had included Medicaid expansion in his previous budget proposal for FY 2020-2021, but the Republican-controlled legislature did not include it in the final budget. Wisconsin covers adults up to 100% FPL in Medicaid but did not adopt the ACA expansion. |
| Wyoming |
A Medicaid expansion bill that passed the Wyoming House for the first time subsequently failed a vote in the Senate Labor, Health, and Social Service Committee in March 2021. However, on October 22, 2021, the legislature’s Joint Revenue Committee reintroduced this legislation ahead of an October special session—the legislation did not advance. The bill would expand Medicaid contingent on the state continuing to receive a 90% federal match assistance percentage (FMAP) for the expansion population and at least 55% for the traditional Medicaid population (a 5 percentage point increase from the traditional match rate of 50%, which is an incentive included in the American Rescue Plan Act for adopting expansion). Prior to the new ARPA incentive, the Wyoming legislature had rejected multiple Medicaid expansion bills during the 2020 and other previous legislative sessions. |