Insulin Out-of-Pocket Costs in Medicare Part D
Addressing the cost of insulin continues to be at the forefront of policy discussions around prescription drugs. Legislation has been introduced in Congress that would cap monthly copayments for insulin products at $35 for people with Medicare and private insurance, require the federal government to negotiate insulin prices, and encourage insulin manufacturers to lower list prices. To inform discussions about these proposals, this analysis updates prior work from KFF on out-of-pocket spending on insulin products by Medicare beneficiaries enrolled in Part D drug plans, along with state-level use and spending data, based on prescription drug event claims data through 2020 from the Centers for Medicare & Medicaid Services (CMS) Chronic Conditions Data Warehouse. Available claims data predate the 2021 introduction of the CMS Part D Senior Savings Model in which enhanced Part D drug plans charge a monthly copayment of no more than $35 for selected insulin products. Therefore, this analysis does not reflect any potential cost savings for Part D enrollees who have enrolled in these plans since 2021.
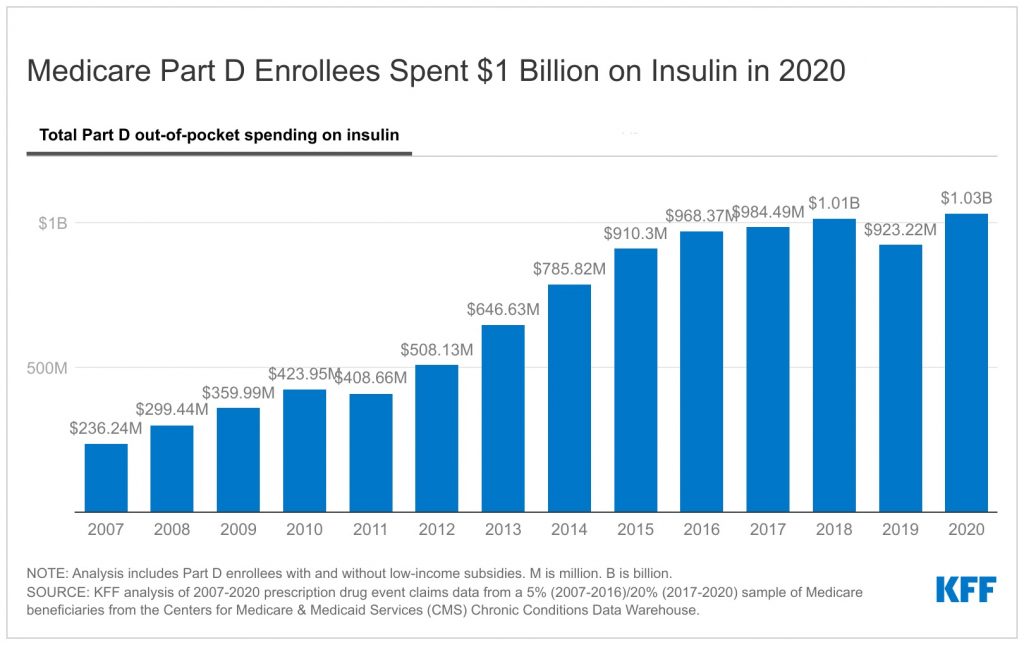
In the aggregate, Part D enrollees spent $1 billion out of pocket on insulin in 2020, more than four times the amount spent in 2007
Aggregate out-of-pocket spending by people with Medicare Part D for insulin products quadrupled between 2007 to 2020, increasing from $236 million to $1.03 billion (Figure 1). The number of Medicare Part D enrollees using insulin doubled over these years, from 1.6 million to 3.3 million beneficiaries, which indicates that the increase in aggregate out-of-pocket spending was not solely a function of more Medicare beneficiaries using insulin.
Average out-of-pocket spending per insulin prescription was $54 in 2020 – over 50% more than the proposed $35 monthly copay cap for insulin – but spending on many insulin products was higher
Among Medicare Part D insulin users who do not receive low-income subsidies, average out-of-pocket costs per prescription across all insulin products was $54 in 2020 – over 50% more than the proposed $35 monthly copay cap for insulin. The $54 per-prescription average in 2020 is an increase of 39% since 2007.
Among all insulin products available in 2020, out-of-pocket spending per prescription by non-LIS Part D enrollees ranged from $16 for Humulin N, an intermediate-acting insulin used by 74,000 non-LIS enrollees in 2020, to $116 for Humulin R U-500, a short-acting concentrated insulin used by 3,600 non-LIS enrollees in 2020 (Figure 2). Some of the more commonly used insulin products with above-average per prescription costs in 2020 include Novolog Mix 70-30 Flexpen ($77 per prescription; used by 32,900 non-LIS enrollees); Tresiba Flextouch U-200 ($70 per prescription; used by 93,700 non-LIS enrollees); and Levemir ($67 per prescription; used by 43,000 non-LIS enrollees).
Among insulin users, Part D enrollees without low-income subsidies spent $572 per person for insulin in 2020, on average, but a small share of insulin users spent considerably more
Among insulin users without Part D low-income subsidies (LIS), average annual out-of-pocket spending on insulin per user increased by 76% between 2007 and 2020, from $324 to $572 (Figure 3; see Table 1 for 2020 insulin use and spending by state). Average annual growth in out-of-pocket costs between 2007 and 2020 was 4.5%, which exceeded the 1.7% average annual rate of growth in inflation over these same years.
Some Part D insulin users spent considerably more than the average in 2020. For example, 10% of non-LIS insulin users spent more than $1,300 on insulin in 2020 and 1% spent more than $2,300 (Figure 4). Higher-than-average out-of-pocket spending is due to a greater number of prescription fills for insulin products and higher out-of-pocket costs per insulin prescription. In other words, taking more than one insulin product and taking more expensive formulations leads to higher out-of-pocket costs.
If insulin copays were capped at $35, Part D enrollees would save 35% on average, based on spending of $54 per prescription in 2020
Policymakers have introduced proposals to cap monthly copayments for insulin products, building on the Part D insulin model. If a $35 monthly copay cap for all insulin products had been in place in 2020, Part D enrollees without low-income subsidies would have saved $19 per insulin prescription, on average—a reduction of 35% based on average out-of-pocket costs of $54 per insulin prescription in 2020.
Under the current Part D insulin model, participating plans are not required to cover all insulin products at the $35 monthly copayment amount, just one of each dosage form (vial, pen) and insulin type (rapid-acting, short-acting, intermediate-acting, and long-acting). Absent a requirement to cover all insulin products at no more than a $35 copay, insulin users might need to switch from one insulin product to another to save on their out-of-pocket costs, or switch to a plan that covers their insulin product at the $35 copayment.
This work was supported in part by Arnold Ventures. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
Juliette Cubanski is with KFF. Anthony Damico is an independent consultant.