Germs Lead the Way: Exploring Microbial Ecology to Elevate the Fight Against Antimicrobial-resistant Healthcare-associated Infections
Three to four billion years ago, microbes (germs) were the first life on earth. They have thrived for millions of years longer than humans have existed. Much like humans, microbes have complex social and physical communities and are always evolving. These microbial communities are home to helpful germs and pathogens (harmful germs). Better understanding the ecology of microbes—relationships within and across these communities—is just the beginning of public health’s scientific journey. We are working to better understand what microbes and their surrounding environments can teach us about preventing infections, including antimicrobial-resistant infections.
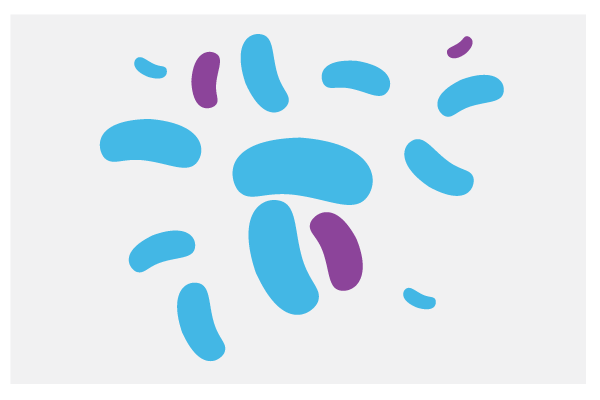
CDC knows there is an important connection between microbial ecology and the health and wellbeing of people. We all have our own microbial communities, called microbiomes, on our skin and in our gut that help us maintain good health. We have a better chance of fighting infections when our microbiomes are in balance—a mix of “good” beneficial germs to help keep the “bad” pathogens in check.
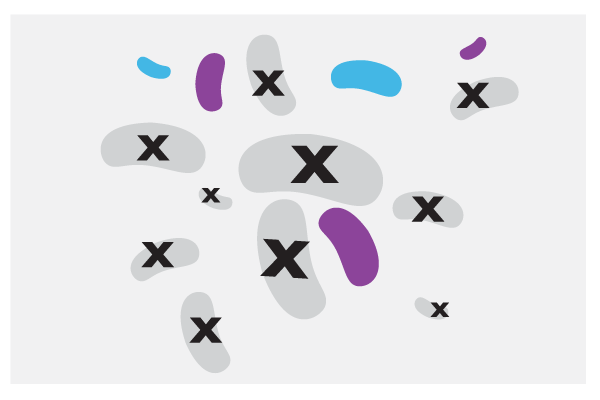
However, when we take antibiotics, antifungals, or other therapeutics, these drugs kill all germs—both the harmful and helpful. This disrupts our microbiome, allowing the surviving pathogens, which are often resistant to the treatment, to dominate our microbiome. This can lead to infection.
Our risk for infection increases when we are colonized, meaning we have a threatening pathogen in our body but do not have symptoms of an infection. Our risk of infection is even higher when we are colonized and have a disrupted microbiome.
Leveraging microbial ecology to advance and protect our health involves a cross-cutting and dynamic effort from diverse collaborators, including public health experts, academic researchers, private industry, and regulatory experts. Expanding our microbial ecology knowledge at the intersection of public health will lead us to new strategies to prevent infections and combat antimicrobial resistance, especially in healthcare settings.
Leveraging Microbial Ecology to Protect Patients
Although scientists know that microbial ecology plays an important role in maintaining human health, there are remaining scientific questions. CDC invests in microbial ecology research to study the interactions of microbes among people, animals, plants, food, and surfaces (e.g., counter tops), all of which can serve as sources of microbes that can lead to infection.
When a healthcare facility identifies certain multidrug-resistant pathogens within their facility, CDC recommends colonization screening—using laboratory test to identify patients who are colonized. When patients are colonized, a unique patient safety intervention called pathogen reduction and decolonization can remove the colonized pathogens in a patient’s microbiome, such as skin, nose, or gut.
Healthcare providers are already using traditional therapeutic strategies to decolonize people, such as antiseptic agents like chlorhexidine gluconate. These strategies help avoid the loss of beneficial germs and disrupting microbiomes because they can:
- Limit application to a certain body site/individual microbiome or specific pathogens
- Decrease the use of antibiotics and antifungals to treat infections, which can help slow antimicrobial resistance
- Focus on colonized individuals or larger populations of patients who are at increased risk for infection
However, more research is needed in the field of microbial ecology to expand upon and develop new therapeutic strategies that address colonization, healthcare-associated infections (HAIs), and antimicrobial resistance, all while considering patient safety and the implications for a patient’s microbiome. This innovative work helps us better understand how to develop and implement life-saving tools.
To expand our patient safety toolbox, CDC needs public health experts, academic researchers, private industry, and regulatory experts to develop preventative products or strategies that:
- Prevent colonization recurrence and do more than “decontaminate,” such as protecting and/or restoring the microbiome
- Reduce pathogen burden (load) and/or eliminate pathogens completely, especially if there is a targeted application (e.g., body site, pathogen)
- Benefit both individuals (individual patients or “source”) and populations
We also need more conversations to continue identifying challenges that arise and form new paths forward as public health and scientific experts explore this untraversed landscape.
How You Can Help

 Consider the impact of antibiotics, antifungals, & other therapeutics on microbiomes when implementing antimicrobial stewardship practices.
Consider the impact of antibiotics, antifungals, & other therapeutics on microbiomes when implementing antimicrobial stewardship practices.
 Incorporate pathogen reduction & decolonization into clinical practice when appropriate.
Incorporate pathogen reduction & decolonization into clinical practice when appropriate.
 Learn about the importance of protecting microbiomes.
Learn about the importance of protecting microbiomes.
 Reduce your & your patient’s risk of HAIs from water in healthcare facilities.
Reduce your & your patient’s risk of HAIs from water in healthcare facilities.
As leaders in public health and patient safety, CDC and the Food and Drug Administration (FDA) are co-sponsoring a public virtual workshop on August 30, 2022, on developing therapeutic drugs for HAIs and the role microbial ecology can play in this effort.
The workshop is the first of its kind to focus on the
- Current state of pathogen-directed products to prevent HAIs
- Decolonization as a strategy to prevent HAIs and their spread
- Targeting antimicrobial-resistant pathogens
- Challenges and approaches to developing drugs and registering products to prevent HAIs
Can’t make the meeting? You can still help!

From policy, industry, academics, funding institutions, and researchers, to healthcare personnel, patients, and advocacy groups—we can all contribute to incorporating microbial ecology into our prevention work. We look forward to working with you and having more conversations together as we enter this new terrain together.
Melia Haile, Christopher Elkins, Cliff McDonald, Alison Laufer Halpin, and Mihnea Mangalea, Division of Healthcare Quality Promotion, and Lacey Avery, Antimicrobial Resistance Coordination and Strategy Unit, National Center for Emerging and Zoonotic Infectious Diseases at the Centers for Disease Control and Prevention (CDC)