COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes Over Time
Over the course of the COVID-19 pandemic, analyses of federal, state, and local data have shown that people of color have experienced a disproportionate burden of cases and deaths. This brief examines racial disparities in COVID-19 cases and deaths and how they have changed over time based on KFF analysis of data on COVID-19 infections and deaths from CDC. It updates a February 2022 analysis to reflect data through mid-2022, amid the ongoing surge associated with the Omicron variant. It finds:
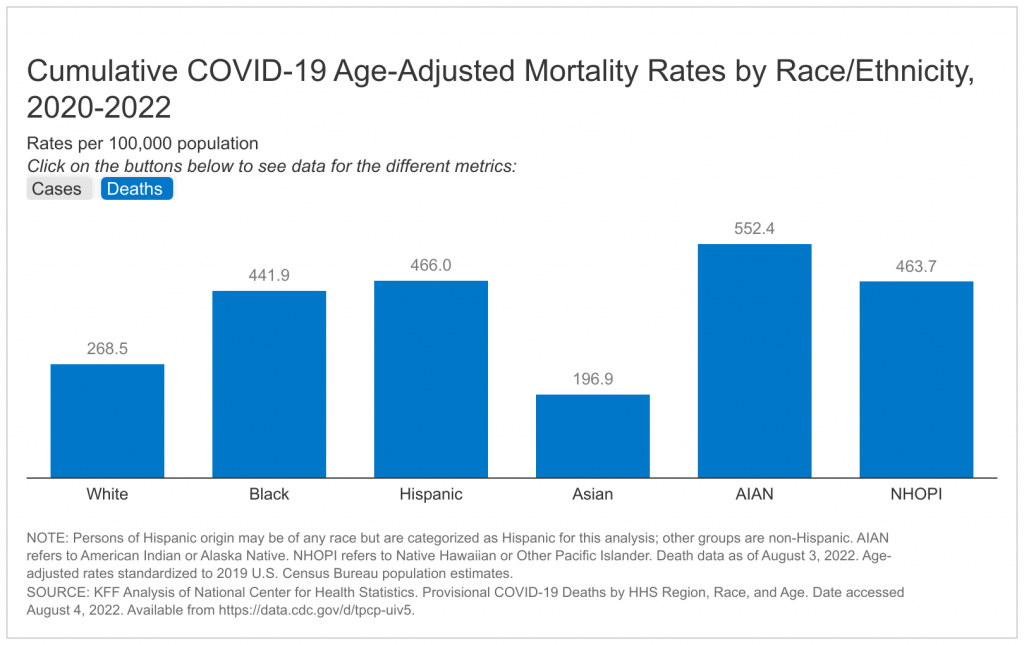
- Total cumulative data show Black, Hispanic, American Indian or Alaska Native (AIAN), and Native Hawaiian or Other Pacific Islander (NHOPI) people have experienced higher rates of COVID-19 cases and deaths compared to White people when data are adjusted to account for differences in age by race and ethnicity.
- Disparities in infections and deaths have both widened and narrowed at various times over the course of the pandemic, with disparities generally widening during periods in which the virus has surged and narrowing when overall infection rates fall. In data that has not been adjusted for age, there were some periods when death rates for White people were higher than or similar to some groups of color. However, in the age-adjusted data, White people have lower death rates than AIAN, Black, and Hispanic people over most of the course of the pandemic and disparities are larger for AIAN, Black, and Hispanic people, reflecting an older White population and higher rates of death across all age groups among people of color compared to White people.
Continuing to assess COVID-19 health impacts by race/ethnicity is important for both identifying and addressing disparities and preventing against further widening of disparities in health going forward. While disparities in cases and deaths have narrowed and widened over time, the underlying structural inequities in health and health care and social and economic factors that placed people of color at increased risk at the outset of the pandemic remain. As such, they may remain at increased risk as the pandemic continues to evolve and for future health threats, such as the Monkeypox virus, for which early data show similar disparities emerging.
Disparities in Total COVID-19 Cases and Deaths
As of August 5, 2022, the Centers for Disease Control and Prevention (CDC) reported a total of over 84 million cases, for which race/ethnicity was known for 65% or over 55 million, and a total of over 880,000 deaths, for which race/ethnicity was known for 85% or over 750,000. These estimates are based on a subset of data for which case-level demographic information has been reported to CDC by state health departments, so they differ from those reported elsewhere. For example, CDC reports a total of over 1 million deaths from COVID as of August 5, 2022. Data on cases also are likely significantly underreported as they do not reflect individuals who test positive on home tests and do not report findings to their public health agency.
Total cumulative data show that Black, Hispanic, AIAN, and NHOPI people have experienced higher rates of COVID-19 cases and deaths than White people when data are adjusted to account for differences in age by race and ethnicity. Age-standardized data show that that NHOPI, Hispanic, and AIAN people are at about one and a half times greater risk of COVID-19 infection than White people, and AIAN, Hispanic, NHOPI, and Black people are about twice as likely to die from COVID-19 as their White counterparts (Figure 1). The CDC also reports large disparities in COVID-19 hospitalizations for AIAN, Black, and Hispanic people. (CDC data does not include separate reporting for NHOPI people.) Adjusting for age when comparing groups on health measures is important because risk of infection, illness, and death can vary by age, and age distribution differs by racial and ethnic group. Age adjustment allows for direct comparison between groups on health measures independent of the age distribution differences. For example, unadjusted rates underestimate racial disparities for COVID-19 deaths, since the White population is older compared to populations of color and COVID-19 death rates have been higher among older individuals. Age adjustment has limited impact on case rates by race and ethnicity, suggesting that age plays a more limited role in risk of infection.
Disparities in Cases and Deaths Over Time
Analysis of monthly data on COVID-19 infections from CDC and deaths from NCHS shows disparities in infections and deaths have both widened and narrowed over the course of the pandemic. During periods in which the virus has surged, disparities have generally widened, while they have narrowed when overall infection rates fall. However, over the course of the pandemic, specific patterns of disparities have varied by race and ethnicity and between cases and deaths.
Trends in Cases
Figure 2 shows age-adjusted monthly data on cases by race and ethnicity between April 2020 and July 2022. There were no notable differences in patterns of disparities between unadjusted and age-adjusted data for reported cases. The data show that during periods of resurgence, disparities have generally widened for people of color compared to White people, while they have narrowed when overall infection rates fall.
- Early in the pandemic Hispanic, AIAN, and Black people had higher rates of COVID-19 cases compared to their White counterparts, with a particularly high rate among Hispanic people. Asian people had the lowest monthly infection rate.
- Case rates increased through Winter 2021, spiking in December 2021, and disparities further widened for Hispanic and AIAN people. Following the spike in December 2021, monthly infection rates fell across all groups. By June 2021, gaps between groups narrowed.
- By August 2021, infection rates rose again across groups, reflecting the spread of the Delta variant, with higher rates for Black and AIAN people compared to White people during this resurgence.
- During January 2022, infections sharply rose again across all groups amidst the spread of the Omicron variant, resulting in the highest case rates recorded since the start of the pandemic. Rates were higher for all groups of color compared to White people, with AIAN people having the highest infection rate during this surge, followed closely by Hispanic people. This surge was also the first time since early in the pandemic that the infection rate for Asian people was comparable to other groups of color. By February 2022, infection rates had fallen sharply, and disparities once again narrowed.
- Between Winter 2022 and June 2022 case rates have fallen across groups. In April, Asian people had the highest infection rate and Black, AIAN and Hispanic people had the lowest infection rate, marking the first time these patterns were observed since the start of the pandemic. More research is needed to understand the factors that contributed to this recent shift in trends. However, by June 2022, this pattern began to reverse with White people having the lowest infection rate, and Hispanic people at highest risk of infection in June and July.
Trends in deaths
Figure 3 presents age-adjusted monthly data on COVID-19 deaths by race and ethnicity between April 2020 and May 2022. Both the unadjusted and age-adjusted data show large disparities in death rates for people of color during surges in the pandemic, with the highest rates among AIAN people for most of the pandemic. In unadjusted data, there were some periods when death rates for White people were higher than or similar to some groups of color. However, in the age-adjusted data, White people have lower death rates than AIAN, Black, and Hispanic people over most of the course of the pandemic and disparities are larger for AIAN, Black, and Hispanic people, reflecting an older White population and higher rates of death across all age groups among people of color compared to White people.
- During the initial surge in summer 2020, AIAN, Hispanic, and Black people experienced higher rates of death than White people. As of July 2020, Hispanic people were five times more likely to die than White people, while AIAN and Black people were roughly four and three times as likely to die than White people, respectively. Asian people were at a similar risk of death as White people.
- Deaths peaked in December 2020 and January 2021 across groups. AIAN and Hispanic people had the highest rates of death, and all groups of color had a higher death rate than White people as of January 2021. Following that surge, death rates fell across all racial and ethnic groups and disparities narrowed by early summer 2021.
- Moving into late summer 2021, amid the rise of the Delta variant, death rates rose and were highest among AIAN people. Black and Hispanic people had higher death rates than White people, while Asian people had the lowest rate of death Following the Delta surge, monthly deaths declined slightly across groups with higher rates of death for AIAN people persisting before climbing again across groups in late 2021 with the arrival of the Omicron variant.
- As of January 2022, during the Omicron surge, Black, AIAN, and Hispanic people experienced the highest rates of death (36.5, 33.1, and 29.4 per 100,000 population, respectively). Following the spike in early 2022, monthly death rates fell across all groups and gaps between groups narrowed with similar rates of death across all groups (2.4 per 100,000 for AIAN and White people, 2.0 per 100,000 for Black people, 1.5 per 100,000 for Hispanic people, and 1.4 per 100,000 for Asian people.)
Discussion
In sum, these data show that, overall, Black, Hispanic, and AIAN people have experienced higher rates of COVID-19 infection and death compared to White people when accounting for age differences across racial and ethnic groups. The age-adjusted data also suggest that while these disparities have narrowed at times over the course of the pandemic, people of color are disproportionately impacted by surges caused by new variants, with disparities widening during these periods.
The higher rates of infection among people of color likely reflect increased exposure risk due to working, living, and transportation situations, including being more likely to work in jobs that cannot be done remotely, to live in larger households, and to rely on public transportation. Black, Hispanic, and AIAN people have experienced the highest age-adjusted death rates amid each resurgence period, reflecting higher rates of death across all age groups among people of color compared to White people and an older White population. Overall, death rates have decreased across groups over the course of the pandemic as vaccination rates have increased and vaccination – particularly with boosters – continues to be highly effective at reducing the risk of hospitalization and death. Early disparities in vaccination rates by race and ethnicity have also narrowed over time. However, data suggest potential disparities in access to COVID-19 treatments, which will be important to monitor going forward.
Looking ahead, continuing to assess COVID-19 health impacts by race/ethnicity is important for both identifying and addressing disparities and preventing against further widening of disparities in health going forward. While disparities in cases and deaths have narrowed and widened during different periods over time, the underlying structural inequities in health and health care and social and economic factors that placed people of color at increased risk at the outset of the pandemic remain. As such, they may remain at increased risk as the pandemic continues to evolve and for future health threats, such as the Monkeypox virus, for which early data show similar disparities emerging.
Methods
This analysis uses data from multiple sources including the Centers for Disease Control and Prevention (CDC) COVID Data Tracker, the Centers for Disease Control and Prevention COVID-19 Response. COVID-19 Case Surveillance Data, the National Center for Health Statistics (NCHS) Provisional COVID-19 Deaths, and the Census Bureau Annual Estimates of the Resident Population. Unless otherwise noted, race/ethnicity was categorized by non-Hispanic White (White), non-Hispanic Black (Black), Hispanic, non-Hispanic American Indian and Alaska Native (AIAN), non-Hispanic Asian (Asian), and non-Hispanic Native Hawaiian or Other Pacific Islander (NHOPI).
Data on COVID-19 infections includes reported cases as of August 1, 2022 and data on COVID-19 deaths includes provisional deaths as of July 30, 2022 where race/ethnicity was available. Age-adjusted infection and death rates were standardized to the 2019 U.S. Census Bureau Annual Estimates of the Resident Population using the direct method of standardization. The direct method of age standardization is calculated by multiplying the age specific crude rates for each population by the appropriate weight in standard population and summing them to produce an age-standardized rate. Data for monthly age adjusted NHOPI cases and deaths not shown due to small number of observations. Age standardization allows for direct comparison of groups on health measures independent of differences in age distribution that may influence the measure being examined.