CDC’s Latest Report: The Top Resistant Pathogens of Concern Spread on Surfaces
 The Centers for Disease Control and Prevention (CDC) recently released a report addressing the impact COVID-19 has had on antimicrobial resistance. While other reports have covered the incidence of hospital-associated infections during COVID, this report focused on the prevalence of drug-resistant strains of the pathogens causing the HAIs. The report reveals that the top drug-resistant pathogens are transmitted via contaminated surfaces, which become reservoirs for these strains that elude our most powerful treatments. In today’s post, we will share their findings and their implications for infection prevention.
The Centers for Disease Control and Prevention (CDC) recently released a report addressing the impact COVID-19 has had on antimicrobial resistance. While other reports have covered the incidence of hospital-associated infections during COVID, this report focused on the prevalence of drug-resistant strains of the pathogens causing the HAIs. The report reveals that the top drug-resistant pathogens are transmitted via contaminated surfaces, which become reservoirs for these strains that elude our most powerful treatments. In today’s post, we will share their findings and their implications for infection prevention.
Let’s start with a look at the big picture impact of COVID-19 on infection prevention. We entered the global pandemic already experiencing growing antimicrobial resistance, and the stress on the medical care system only made it worse. One of the major drivers of antimicrobial resistance is the over-prescription of antibiotics, a practice which accelerated during the pandemic as doctors responded to symptoms and illness with antibiotics which had no impact on the virus. Additionally, as healthcare facilities were overwhelmed with COVID-19 patients, their ability to follow infection prevention protocols was compromised. Finally, with so much effort required to track and report COVID-19 tests, cases, and outcomes, tracking hospital-associated infections fell to the wayside. All these factors resulted in a 15% increase in resistant hospital-onset infections and deaths during the first year of the pandemic, essentially undoing the 18% reductions that were seen prior to 2020.
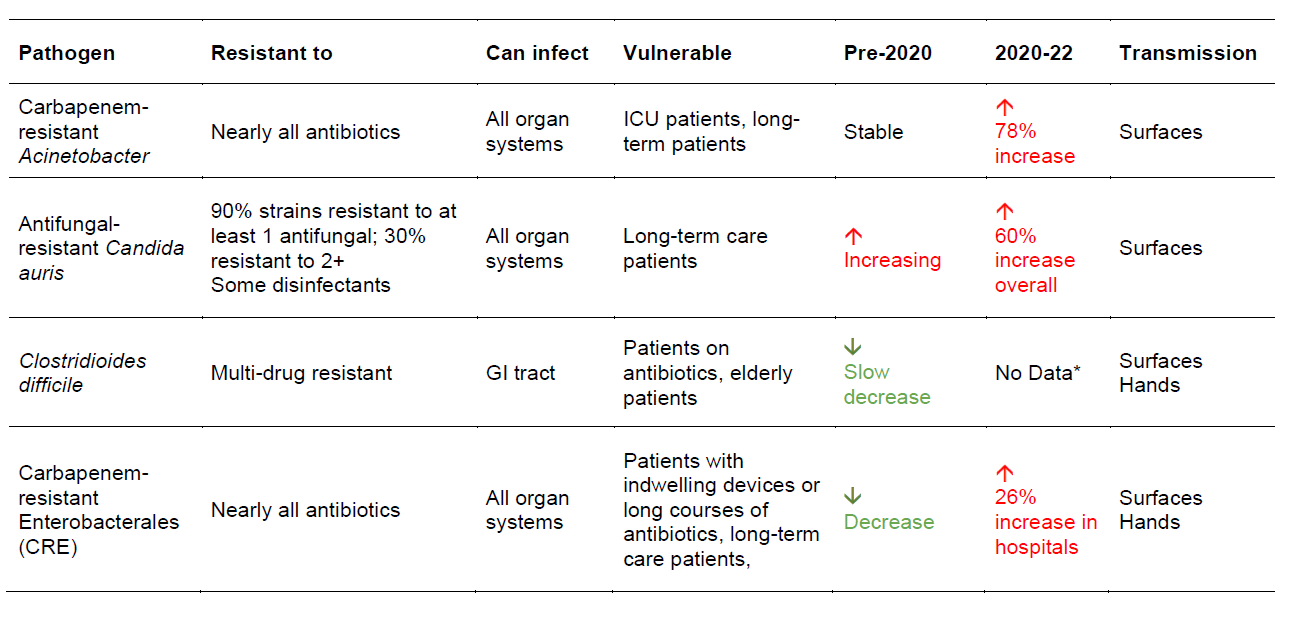
The CDC report presented the data on the pathogens of greatest concern in the context of their degree of resistance, who is at greatest risk, the trend in infections before the pandemic, and the impact of COVID-19. Here are their findings for the most urgent hospital-associated pathogens:
* Based on other data collected by the CDC, it is possible that there was a decrease in C. diff infections during the pandemic.
In the infographic linked below, you can see the results on the serious and concerning pathogens,
most of which show significant increases during the years of the pandemic.
The CDC includes in their report what they see as next steps to reclaiming some of the progress made prior to the pandemic. Their solutions fall under two categories: Reducing antibiotic resistance and reducing hospital-associated infections. To reduce resistance, the number one priority is returning to a focus on antibiotic stewardship, the emphasis on using antibiotics only when necessary and at the lowest appropriate dose. To reduce hospital-associated infections, the CDC expects improvement once screening for colonization returns to normal levels (testing resources were heavily curtailed to enable COVID-19 testing), along with a return to normal surveillance and data collection, with increased capacity enabled by the American Rescue Plan Act of 2021. Education programs, such as through Project Frontline, will provide training in infection prevention to a variety of patient-facing personnel. Research into resistance and vaccines is also underway.
Among the CDC’s public health actions, the report states the “need for more prevention products… to stop infections before they happen.” Prevention is the best way to protect vulnerable patients. One of the more important preventive measures involves decolonization, that is, removing the pathogens found on the skin of patients before they get a chance to reach a surface, a wound, an indwelling device, or hand. As total decolonization is not possible, removing contamination from the surfaces surrounding the patient – “decolonizing” the surface” – provides an essential layer of protection. The use of biocidal surface materials continuously kills those pathogens – including MDROs – before they have a chance to infect a vulnerable patient. Equally important, these biocidal materials should not themselves contribute to resistance! Pathogens can become resistant to some disinfectants and cleaners. Copper and copper-infused polymers such as EOScu are the only preventive biocidal surfaces proven to kill these resistant pathogens. Thankfully, they also do not contribute to resistance (read more about that here).
What was your experience with HAIs during the COVID pandemic? Share your experiences below!