An Overview of the Medicare Part D Prescription Drug Benefit
Medicare Part D is a voluntary outpatient prescription drug benefit for people with Medicare provided through private plans that contract with the federal government. Beneficiaries can choose to enroll in either a stand-alone prescription drug plan (PDP) to supplement traditional Medicare or a Medicare Advantage plan, mainly HMOs and PPOs, that provides all Medicare-covered benefits, including prescription drugs (MA-PD). In 2022, 49 million of the 65 million people covered by Medicare are enrolled in Part D plans. This fact sheet provides an overview of the Medicare Part D program, plan availability, enrollment, and spending and financing, based on data from the Centers for Medicare & Medicaid Services (CMS), the Congressional Budget Office (CBO), and other sources. It also provides an overview of upcoming changes to the Part D benefit based on provisions in the Inflation Reduction Act.
Medicare Prescription Drug Plan Availability in 2023
In 2023, 801 PDPs will be offered across the 34 PDP regions nationwide (excluding the territories), a 5% increase from 2022 (Figure 1).
Beneficiaries in each state will have a choice of multiple stand-alone PDPs, ranging from 19 PDPs in New York to 28 PDPs in Arizona (Figure 2). In addition, beneficiaries will be able to choose from among multiple MA-PDs available at the local level.
In 2023, under a provision in the Inflation Reduction Act, Part D enrollees will pay no more than $35 per month for covered insulin products in all Part D plans. This new requirement builds on a current Innovation Center model in which only participating enhanced Part D plans cover insulin products at a monthly copayment of $35 in the deductible, initial coverage, and coverage gap phases of the Part D benefit. In 2023, a total of 2,881 Part D plans will participate in this model, including 324 PDPs and 2,557 MA-PDs. While this model will continue in 2023, beneficiaries will not need to enroll in one of the model-participating plans to benefit from the $35 monthly copay cap for insulin. Under the new Inflation Reduction Act requirement, all Part D plans do not have to cover all insulin products at the $35 monthly copayment amount, only those insulin products that are covered on a plan’s formulary.
Low-Income Subsidy Plan Availability in 2023
Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing. Through the Part D Low-Income Subsidy (LIS) program, additional premium and cost-sharing assistance is available for Part D enrollees with low incomes (less than 150% of poverty, or $20,395 for individuals/$27,465 for married couples in 2022) and modest assets (up to $15,510 for individuals/$30,950 for couples in 2022).
In 2023, 191 plans will be available for enrollment of LIS beneficiaries for no premium, a 4% reduction or 7 fewer benchmark plans compared to 2022 (Figure 3). Just under one-fourth of PDPs in 2022 (24%) are benchmark plans.
Some enrollees have fewer benchmark plan options than others because benchmark plan availability varies at the Part D region level. The number of premium-free PDPs in 2023 ranges across states from 3 to 8 plans (Figure 4). LIS enrollees can select any plan offered in their area, but if they are enrolled in a non-benchmark plan, they may be required to pay some portion of their plan’s monthly premium.
Part D Plan Premiums and Benefits in 2023
Premiums
The 2023 Part D base beneficiary premium – which is based on bids submitted by both PDPs and MA-PDs and is not weighted by enrollment – is $32.74, a modest (2%) decrease from 2022. But actual premiums paid by Part D enrollees vary considerably. For 2023, PDP monthly premiums range from a low of $1.60 for a PDP in the Oregon/Washington region to a high of $201.10 for a PDP in South Carolina (unweighted by plan enrollment). Even within a state, PDP premiums can vary; for example, in Florida, monthly premiums range from $8.40 to $170.10. In addition to the monthly premium, Part D enrollees with higher incomes ($97,000/individual; $194,000/couple) pay an income-related premium surcharge, ranging from $12.20 to $76.40 per month in 2023 (depending on income).
Benefits
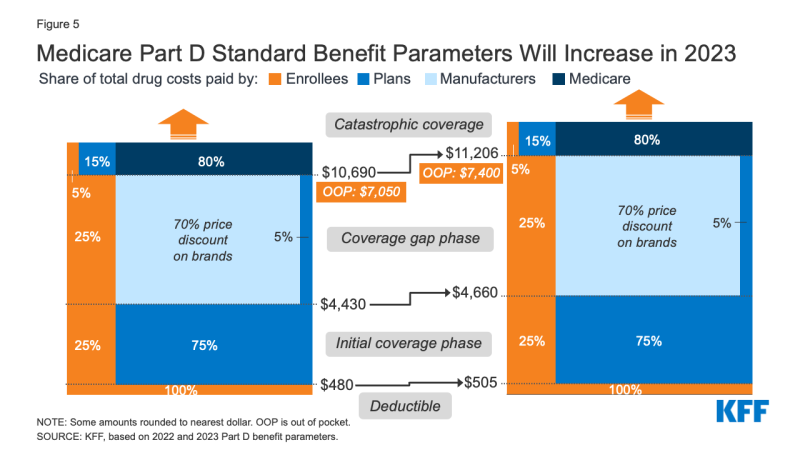
The Part D defined standard benefit has several phases, including a deductible, an initial coverage phase, a coverage gap phase, and catastrophic coverage, although it currently does not have a hard cap on out-of-pocket spending. Between 2022 and 2023, the parameters of the standard benefit are rising, which means Part D enrollees will face higher out-of-pocket costs for the deductible and in the initial coverage phase, as they have in prior years, and will have to pay more out-of-pocket before qualifying for catastrophic coverage (Figure 5).
- The standard deductible is increasing from $480 in 2022 to $505 in 2023
- The initial coverage limit is increasing from $4,430 to $4,660, and
- The out-of-pocket spending threshold is increasing from $7,050 to $7,400 (equivalent to $11,206 in total drug spending in 2023, up from $10,690 in 2022).
The standard benefit amounts are indexed to change annually based on the rate of Part D per capita spending growth, and, except for 2014, have increased each year since 2006.
For costs in the coverage gap phase, beneficiaries pay 25% for both brand-name and generic drugs, with manufacturers providing a 70% discount on brands and plans paying the remaining 5% of brand drug costs, and plans paying the remaining 75% of generic drug costs. For total drug costs above the catastrophic threshold, Medicare pays 80%, plans pay 15%, and enrollees pay either 5% of total drug costs or $4.15/$10.35 for each generic and brand-name drug, respectively.
Part D plans must offer either the defined standard benefit or an alternative equal in value (“actuarially equivalent”) and can also provide enhanced benefits. Both basic and enhanced benefit plans vary in terms of their specific benefit design, coverage, and costs, including deductibles, cost-sharing amounts, utilization management tools (i.e., prior authorization, quantity limits, and step therapy), and formularies (i.e., covered drugs). Plan formularies must include drug classes covering all disease states, and a minimum of two chemically distinct drugs in each class. Part D plans are required to cover all drugs in six so-called “protected” classes: immunosuppressants, antidepressants, antipsychotics, anticonvulsants, antiretrovirals, and antineoplastics.
Changes to Part D Under the Inflation Reduction Act
With the passage of the Inflation Reduction Act, which includes several provisions to lower prescription drug spending by Medicare and beneficiaries, major changes are coming to the Medicare Part D program. These provisions will phase in over the next several years starting in 2023. The law:
- authorizes the Secretary of the Department of Health and Human Services to negotiate the price of some drugs covered under Medicare, with negotiated prices first available for 10 Part D drugs in 2026
- requires drug manufacturers to pay a rebate to the federal government if prices for drugs covered under Part D and Part B increase faster than the rate of inflation, with the initial period for measuring Part D drug price increases running from October 2022-September 2023
- adds a hard cap on out-of-pocket drug spending under Part D by eliminating the 5% coinsurance requirement for catastrophic coverage in 2024 and capping out-of-pocket spending at $2,000 in 2025
- shifts more of the responsibility for catastrophic coverage costs to Part D plans and drug manufacturers, starting in 2025
- limits the price of insulin products to no more than $35 per month in all Part D plans and makes adult vaccines covered under Part D available for free, as of 2023, and
- expands eligibility for full benefits under the Part D Low-Income Subsidy program in 2024.
CBO estimates that the drug pricing provisions in the law will reduce the federal deficit by $237 billion over 10 years (2022-2031).
Part D and Low-Income Subsidy Enrollment
Enrollment in Medicare Part D plans is voluntary, except for beneficiaries who are eligible for both Medicare and Medicaid and certain other low-income beneficiaries who are automatically enrolled in a PDP if they do not choose a plan on their own. Unless beneficiaries have drug coverage from another source that is at least as good as standard Part D coverage (“creditable coverage”), they face a penalty equal to 1% of the national average premium for each month they delay enrollment.
In 2022, 49 million Medicare beneficiaries are enrolled in Medicare Part D plans, including employer-only group plans; of the total, 53% are enrolled in MA-PDs and 47% are enrolled in stand-alone PDPs (Figure 6). Another 1.0 million beneficiaries are estimated to have drug coverage through employer-sponsored retiree plans where the employer receives a subsidy from the federal government equal to 28% of drug expenses between $505 and $10,350 per retiree (in 2023). Several million beneficiaries are estimated to have other sources of drug coverage, including employer plans for active workers, FEHBP, TRICARE, and Veterans Affairs (VA). Roughly 10% of people with Medicare are estimated to lack creditable drug coverage.
Nearly 13 million Part D enrollees receive the Low-Income Subsidy in 2022. Beneficiaries who are dually eligible, QMBs, SLMBs, QIs, and SSI-onlys automatically qualify for the additional assistance, and Medicare automatically enrolls them into PDPs with premiums at or below the regional average (the Low-Income Subsidy benchmark) if they do not choose a plan on their own. Other beneficiaries are subject to both an income and asset test and need to apply for the Low-Income Subsidy through either the Social Security Administration or Medicaid.
Part D Spending and Financing
Part D Spending
The Congressional Budget Office (CBO) estimates that spending on Part D benefits will total $119 billion in 2023, representing 14% of net Medicare outlays (net of offsetting receipts from premiums and state transfers). Part D spending depends on several factors, including the total number of Part D enrollees, their health status and drug use, the number of high-cost enrollees (those with drug spending above the catastrophic threshold), the number of enrollees receiving the Low-Income Subsidy, and plans’ ability to negotiate discounts (rebates) with drug companies and preferred pricing arrangements with pharmacies, and manage use (e.g., promoting use of generic drugs, prior authorization, step therapy, quantity limits, and mail order).
Part D Financing
Financing for Part D comes from general revenues (74%), beneficiary premiums (15%), and state contributions (11%). The monthly premium paid by enrollees is set to cover 25.5% of the cost of standard drug coverage. Medicare subsidizes the remaining 74.5%, based on bids submitted by plans for their expected benefit payments. Higher-income Part D enrollees pay a larger share of standard Part D costs, ranging from 35% to 85%, depending on income.
Payments to Plans
For 2023, Medicare’s actuaries estimate that Part D plans will receive direct subsidy payments averaging $106 per enrollee overall, $2,855 for enrollees receiving the LIS, and $1,140 in reinsurance payments for very high-cost enrollees; employers are expected to receive, on average, $557 for retirees in employer-subsidy plans. Part D plans also receive additional risk-adjusted payments based on the health status of their enrollees, and plans’ potential total losses or gains are limited by risk-sharing arrangements with the federal government (“risk corridors”).
Under reinsurance, Medicare currently subsidizes 80% of total drug spending incurred by Part D enrollees with relatively high drug spending above the catastrophic coverage threshold. In the aggregate, Medicare’s reinsurance payments to Part D plans now account for close to half of total Part D spending (47%), up from 14% in 2006 (increasing from $6 billion in 2006 to $52 billion in 2021) (Figure 7). Higher benefit spending above the catastrophic threshold is a result of several factors, including an increase in the number of high-cost drugs, drug price increases, and a change made by the ACA to count the manufacturer discount on the price of brand-name drugs in the coverage gap towards the out-of-pocket threshold for catastrophic coverage; this change has led to more Part D enrollees with spending above the catastrophic threshold over time.
Issues for the Future
Since its inception, the Medicare drug benefit has helped to limit growth in average out-of-pocket drug spending by Medicare beneficiaries enrolled in Part D plans. More recently, however, a combination of factors, including rising drug prices, more plans charging coinsurance rather than flat copayments for covered brand-name drugs, and annual increases in the out-of-pocket spending threshold, has increased the out-of-pocket cost burden faced by some enrollees, especially those with high drug costs.
Provisions in the Inflation Reduction Act that will be rolling out over the next several years are designed to address several concerns related to Part D, including the lack of a hard cap on out-of-pocket spending for Part D enrollees; the inability of the federal government to negotiate drug prices with manufacturers; the significant increase in Medicare spending for Part D enrollees with high drug costs; prices for many Part D covered drugs rising faster than the rate of inflation; and the relatively weak financial incentives faced by Part D plan sponsors to control high drug costs. Understanding how well Part D continues to meet the needs of people on Medicare as the law’s various provisions are implemented will be informed by ongoing analysis of the Part D plan marketplace, formulary coverage and costs for new and existing medications, and trends in Medicare beneficiaries’ out-of-pocket drug spending.