American Hospital Association Slams ‘Unworkable’ Unified Post-Acute Payment Model Draft
A draft version of Medicare’s unified post-acute care payment model dropped earlier this month. Already, health care stakeholders are describing the plan as an “unworkable” model with “numerous fundamental flaws.”
The U.S. Centers for Medicare & Medicaid Services (CMS), along with the Assistant Secretary for Planning and Evaluation (ASPE), were charged with developing a universal, site-neutral payment model for post-acute care (PAC) settings as part of the Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014. To do so, the two federal agencies teamed up with contractor RTI International.
RTI released its most recent unified PAC payment model draft on July 7.
PAC settings include home health agencies, skilled nursing facilities (SNFs), in-patient rehabilitation facilities (IRFs) and long-term care hospitals (LTCHs). The Medicare fee-for-service (FFS) program spent $57 billion on those services in 2019, with each PAC setting currently under its own payment system, despite often sharing several commonalities.
“Each of the four PAC settings has its own statutory payment system for paying providers for the care they deliver to Medicare FFS patients,” the RTI wrote in the 106-page draft. “As a result, Medicare payments for patients with similar characteristics treated in different PAC settings can vary for reasons independent of patient need.”
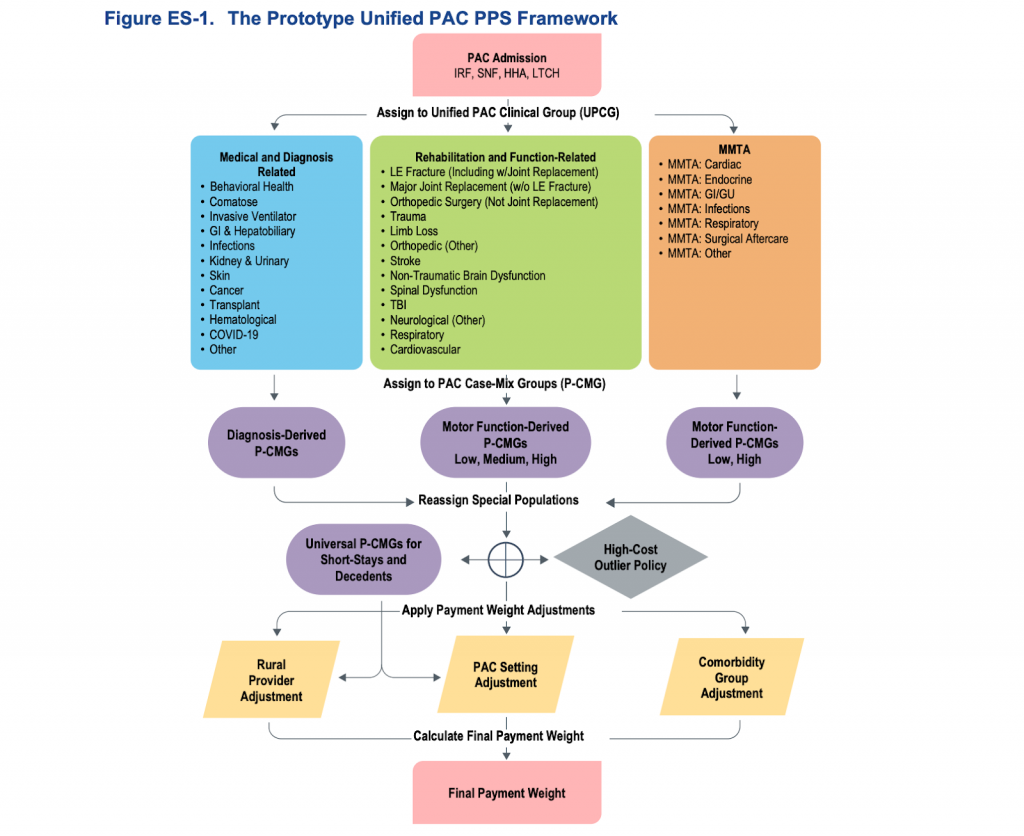
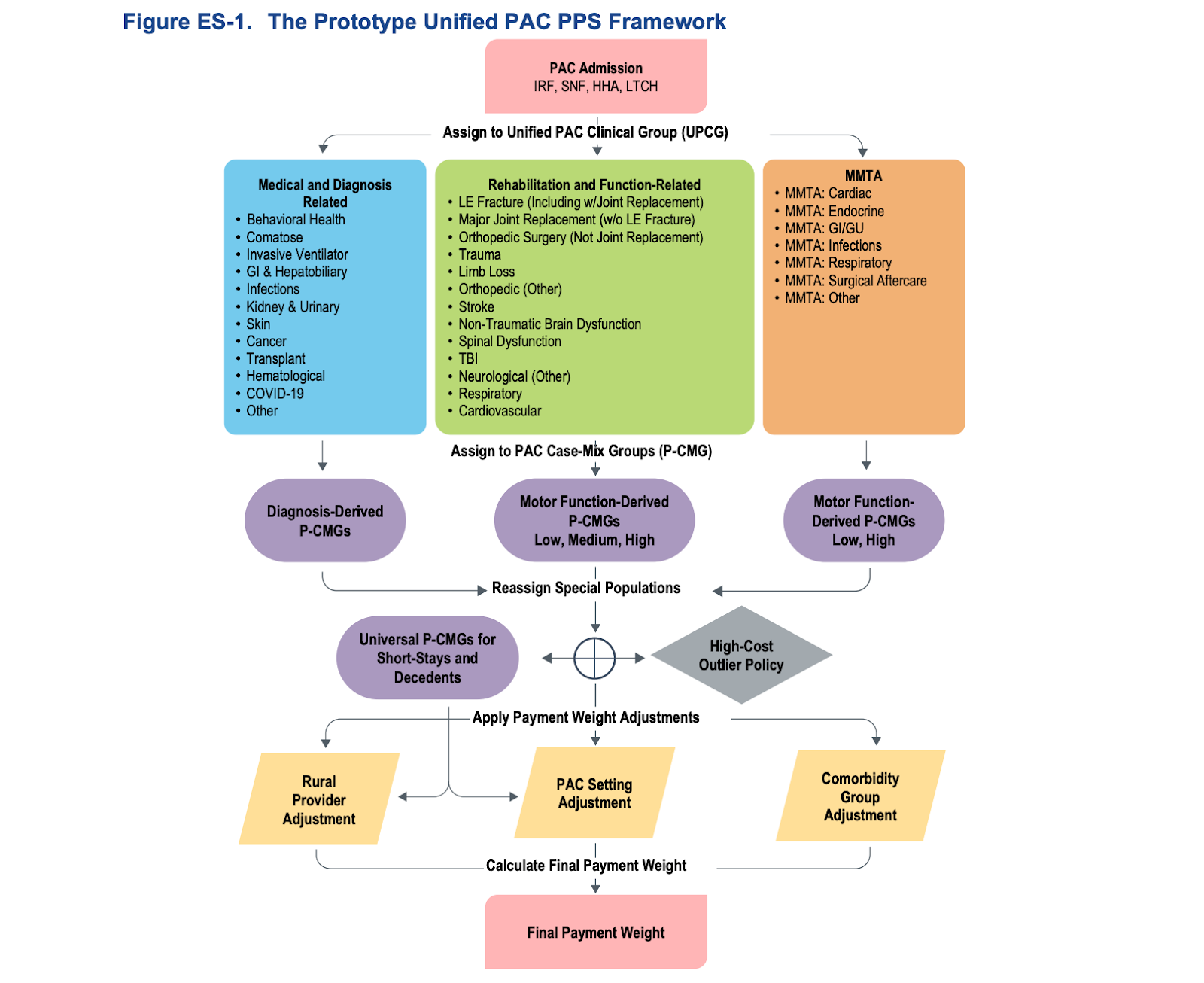
Broadly, the RTI draft bases payment on several key factors relevant to Medicare beneficiary needs and costs of care. These include:
– 32 distinct clinical condition groups, or Unified PAC Clinical Groups (UPCG), representing the patient’s primary reason for PAC
– Subgroups within each UPCG differentiating patients’ needs on the basis of clinical characteristics and relative costliness, with examples being “prior acute stay” and mobility function
– Co-morbidity scoring, or a measure of “how clinically complex” each patient is
– PAC setting types
– Location, specifically whether providers are located in rural areas
The American Hospital Association (AHA) is among the health care groups that have come out swinging against the unified PAC payment model draft.
Among its flaws, AHA says the draft lacks a workable risk-adjustment approach and is missing reforms outlined by CMS.
“Importantly, the draft model lacks a comprehensive and reliable risk adjustment approach, which endangers access to care — particularly for the most critically ill patients,” AHA Executive Vice President Stacy Hughes said in a statement. “It also fails to reflect both the significant reforms that CMS itself has made to the existing PAC payment systems, as well as the fundamental and long-lasting delivery system changes created by the COVID-19 pandemic.”
RTI’s draft is based on pre-pandemic data.
Because of that, AHA points out that the draft design is largely based on “out-of-date patient utilization patterns and patient care protocols.”
“Additionally, the draft model identifies patients’ clinical characteristics using inconsistent definitions and guidelines,” Hughes noted.
Even CMS and ASPE acknowledge their draft model still needs significant work.
“Although we believe that the clinical concepts and analytic approach upon which the prototype is based are sound, it will be important to understand the implications for costs of care of COVID-19 and the revised payment systems, and to recalibrate the payment weights accordingly,” they said in their report to Congress.
Other factors like unified cost-sharing rules and the value-based purchasing (VBP) program will need to be considered too, according to CMS, ASPE and RTI.
“The agencies should go back to the drawing board to create a solution that both reflects the current health care delivery system and ensures access to care for all Medicare PAC patients,” said Hughes.
Additional reporting by Amy Stulick