After Roe: Options to Address Medicaid Coverage Policy Related to Maternal and Child Health
The Supreme Court decision overturning Roe v. Wade turned the spotlight on state abortion policies and the health and economic wellbeing of women and children across states. With Medicaid covering 42% of births in the U.S., it’s a key part of the equation when it comes to maternal and child health.
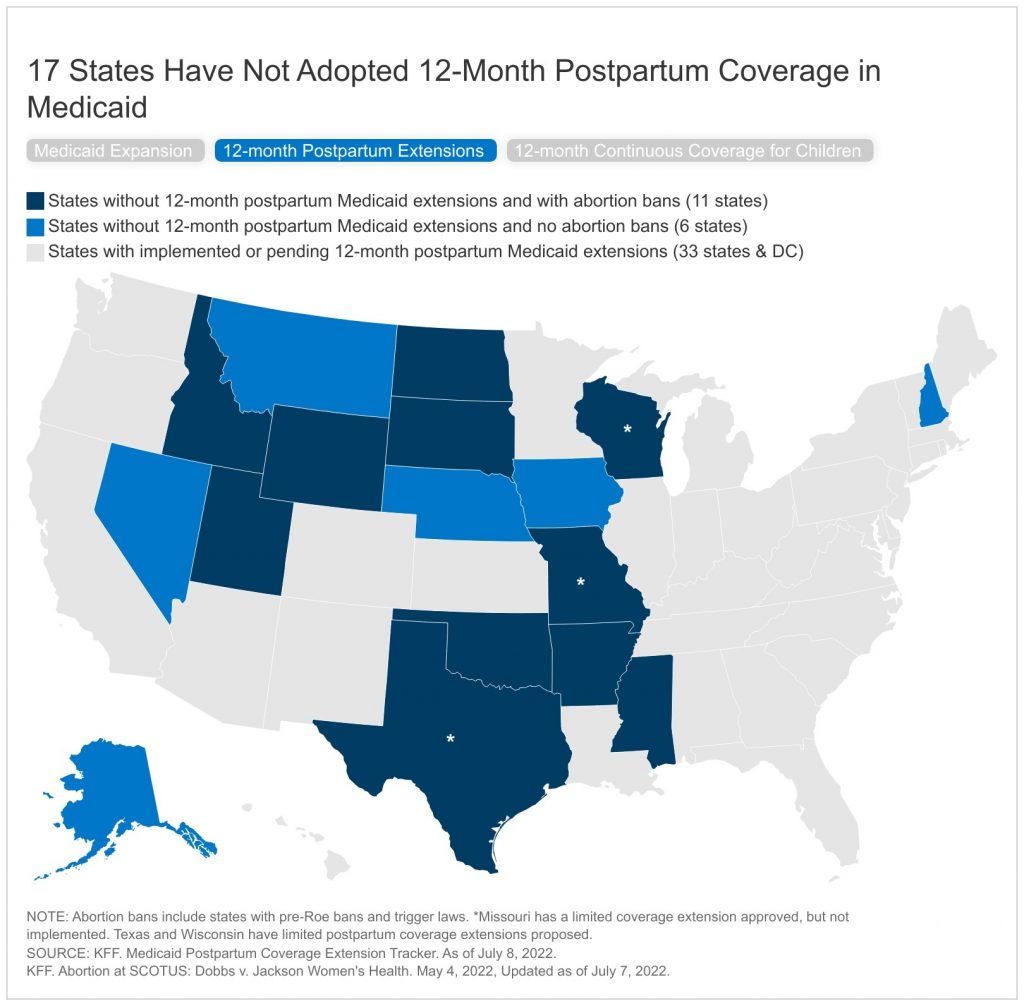
While there has been federal legislation enacted to encourage states to improve maternal and child health, address health disparities and expand Medicaid coverage, there has been variation in state uptake of these options. For example, while the American Rescue Plan Act (ARPA) included a new option for states to adopt 12-month postpartum coverage and new incentives for states to newly adopt the Medicaid expansion, a number of states have not yet taken up these options. The Build Back Better Act (BBBA), adopted by the House of Representatives in November 2021, included a number of provisions to expand coverage for Medicaid by closing the Medicaid coverage gap and requiring states to extend postpartum coverage to 12 months and to provide 12-month continuous coverage for children, along with other maternal health provisions. There are active discussions in the Senate about the shape of a budget reconciliation bill, which is expected to include very limited health spending provisions.
The outcome of the recent court decision overturning Roe v. Wade re-elevates the implications and importance of coverage policies that affect low-income women and children. While extending Medicaid coverage to low-income parents and stabilizing coverage for their children is not a replacement for abortion access, a pathway to stable coverage could expand access to care to those who could be impacted by the abortion bans. This policy watch examines the intersection of these Medicaid coverage policies with state actions to ban abortion.
Medicaid is the primary source of coverage for low-income pregnant people and children. In 2020, Medicaid covered 16% of nonelderly adult women in the United States, but Medicaid coverage rates were higher among certain groups, including women in fair or poor health, women of color, single mothers, low-income women, and women who have not completed a high school education. These are also similar to the demographics for women who get abortions in the US: 75% have household incomes below 200% of the federal poverty level, 61% are women of color, 72% are under age 30, and 59% already have had a prior birth. Medicaid currently finances the cost of 42% of births in the U.S. and in a number of states the share is 50% or greater. With abortion bans in place in a number of states, this share could increase, as low-income women are less likely to have the ability to travel to another states to access an abortion because they can’t afford to travel, or have jobs with limited flexibility or time off, and limited options for child care.
Research has shown that Medicaid expansion has helped to improve maternal and infant health, postpartum insurance coverage, and access to contraception. In addition, research shows that Medicaid expansion was associated with narrowed disparities in health outcomes for Black and Hispanic individuals, particularly for measures of maternal and infant health. Under current law, the federal government pays for 90% of the costs of expansion, but the American Rescue Plan Act (ARPA) included an additional temporary fiscal incentive for states that newly adopt the Medicaid expansion. The House-passed budget reconciliation bill would create a federal provision to close the coverage gap by allowing people living in states that have not expanded Medicaid to temporarily purchase subsidized coverage on the ACA Marketplace. Of the 12 states that have not adopted the Medicaid expansion, seven have abortion bans in place (AL, MS, SD, TN, TX, WI and WY) (Figure 1). Most of these states have eligibility levels for parents in Medicaid below 50% of the federal poverty level ($11,515 annually for a family of three in 2022), so many could become uninsured at the end of the 60-day postpartum coverage period. In Texas and Alabama, the eligibility threshold for parents is below 20% of the poverty level.
Adopting the Medicaid postpartum coverage extension can help to improve maternal health and coverage stability and help address racial disparities in maternal health. A provision in ARPA gives states a new option to extend Medicaid postpartum coverage to 12 months, with the federal government and states sharing in the cost. While this new option took effect on April 1, 2022 and is available to states for five years, 17 states have not adopted (or have plans) the 12-month postpartum coverage extension. Texas and Wisconsin have proposed limited postpartum coverage extensions, and Missouri has indicated to CMS that it will not implement its approved but limited six-month postpartum extension – these states are included in the 17 states. Eleven of those 17 states have passed abortion bans (Figure 1). The House-passed budget reconciliation bill would require 12 months of postpartum coverage in all states, at a federal cost of $1.2 billion over a decade.
While states have the option to provide 12-month continuous coverage for children in Medicaid and CHIP, many have not done so. As of January 2022, 32 states have opted to provide 12-month continuous eligibility for all children in Medicaid and/or CHIP. The continuous coverage policy for children is more common in CHIP, with 24 of 34 separate CHIP programs providing a full year of coverage compared to 24 of the 51 Medicaid programs that have adopted the option. Continuous eligibility eliminates coverage gaps due to income fluctuations, which are often temporary, and is referenced in recent CMS guidance as a strategy for promoting continuous coverage for eligible individuals and reducing churn, when individuals go on and off the program. Of the 18 states and DC that have not adopted 12-month continuous coverage for children, six have abortion bans in place (Figure 1). The House-passed budget reconciliation bill did not have a separate cost estimate for the provision to require 12-month continuous coverage for children.
The state bans will further limit abortion access or even make it effectively impossible for low-income women who live in most states in the South and Midwest. Many of the very states that have banned abortion have not taken advantage of current federal options to strengthen health coverage for their state residents, most notably for women who give birth and children. The recent court decision to overturn Roe v. Wade renews the focus and attention on maternal and child health as states implement abortion bans.