As 2022 Legislative Sessions End, Most States Are Adopting New Option to Extend Medicaid Postpartum Coverage
Earlier this year, a temporary option to extend Medicaid postpartum coverage from 60 days to 12 months took effect. This option, included in the American Rescue Plan Act (ARPA), is part of a broader federal and state effort to address racial disparities and improve maternal and infant health outcomes. Medicaid is a key source of coverage for low-income women in the United States and covers more than four in ten births nationally. Research has documented the importance of having continuous Medicaid coverage following pregnancy to ensure access to needed care during the postpartum period, such as follow up on pregnancy complications, management of chronic health and mental health conditions, and access to family planning services. There has been, however, a history of considerable churning off the program in the postpartum period, especially among women who live in states that have not expanded Medicaid eligibility under the Affordable Care Act (ACA). KFF research has found four in ten pregnant people are disenrolled from Medicaid coverage after giving birth and if all states had adopted the postpartum extension in 2018, over 610,000 individuals who were disenrolled during the postpartum year would have been able to retain coverage.
The Supreme Court decision overturning Roe v. Wade has also refocused attention on the importance of coverage for pregnancy and postpartum care along with other maternal and child health programs. This policy watch provides an update on the status of state adoption and implementation of the Medicaid 12-month postpartum coverage extension option as states wrap up their 2022 legislative sessions.
Prior to the ARPA option, postpartum coverage was limited to 60 days. Under federal law, states must cover pregnant individuals with incomes up to at least 138% of the federal poverty level (FPL), although many states have set higher income eligibility levels, and they must extend coverage for 60-days postpartum. Following the 60-day postpartum period, in states that have adopted the Affordable Care Act (ACA)’s Medicaid expansion, individuals with incomes below 138% FPL may continue to be eligible for Medicaid coverage. Those with income above the federal poverty level may qualify for subsidized coverage through the ACA marketplace plans; however, individuals in the remaining 12 non-expansion states may become uninsured because their income is too high to qualify for Medicaid as a parent but too low to qualify for subsidized Marketplace plans. This group falls into what is called the “Medicaid coverage gap.” For example, in Mississippi, which has not sought a postpartum coverage extension nor the ACA’s Medicaid expansion, the Medicaid eligibility level for parents is 25% FPL, which is approximately $5,758/year for a family of three.
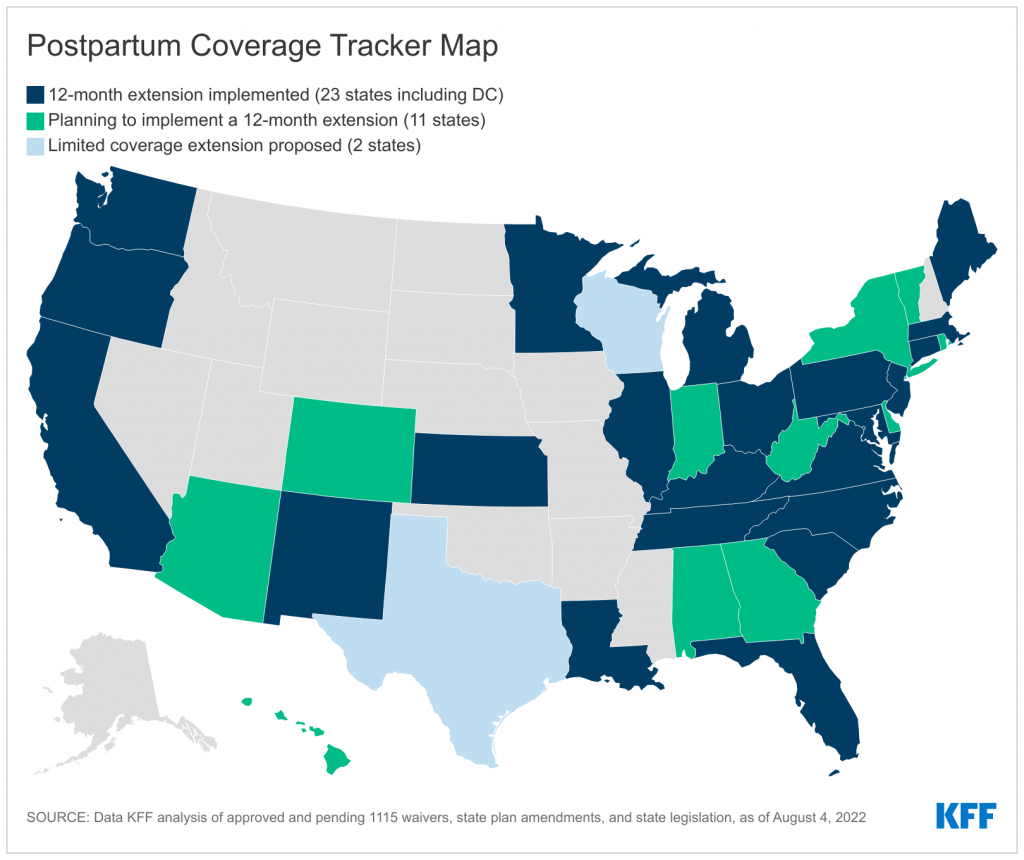
Two-thirds of states (34 including DC) have extended or have plans to extend Medicaid postpartum coverage to 12 months. Recent state actions related to 12-month postpartum coverage include the following:
- 15 states (CA, CT, DC, KY, KS, LA, MA, ME, MI, MN, NM, OR, TN, SC, & WA) received state plan amendment (SPA) approvals ;
- 4 states (MD, NC, OH, and PA) announced that coverage extension has taken effect, although CMS has not yet approved the SPAs in these states;
- 11 states (AL, AZ, CO, DE, GA, HI, IN, NY, RI, VT, & WV) are planning to implement;
- 4 states (FL, IL, NJ, VA) received Section 1115 waiver approvals.
Although states can now implement this coverage extension, postpartum coverage has been continuous during the COVID-19 public health emergency as Medicaid disenrollments have been suspended across the country in exchange for enhanced federal matching dollars. Once the public health emergency is lifted, however, this coverage will no longer be available.
Two states are seeking limited postpartum coverage extensions. Wisconsin submitted a Section 1115 waiver proposal that would extend coverage from 60 days to 90 days and Texas submitted a waiver proposal that would extend coverage to six months, with the additional four months of coverage limited to individuals who “deliver or involuntarily miscarry” only. CMS has not issued a decision on either proposal. Missouri had received CMS approval for a limited 12-month extension to postpartum individuals with substance use disorders, but the state has paused implementation of this coverage extension.
Among the 17 states not taking up the full postpartum extension, a number have not adopted the ACA Medicaid expansion and/or have banned abortion. Of these states, five (MS, SD, TX, WI, WY) have also not adopted the Medicaid expansion. After the PHE is lifted, postpartum enrollees in these states would be at particularly high risk for losing coverage just two months after their pregnancy ends. Additionally, 11 of the 17 states (AR, ID, MS, MO, ND, OK, SD, TX, UT, WI, WY) have banned abortion or have abortion bans that may soon take effect. While extending Medicaid coverage to postpartum parents is not a replacement for abortion access, a pathway to stable coverage could ensure access to care to those who could be affected by the abortion bans and improve access to care during a time of medical vulnerability for many.
To track updated state-by-state activity on Medicaid postpartum coverage, please visit our Medicaid Postpartum Coverage Extension Tracker.