Analysis of Recent National Trends in Medicaid and CHIP Enrollment
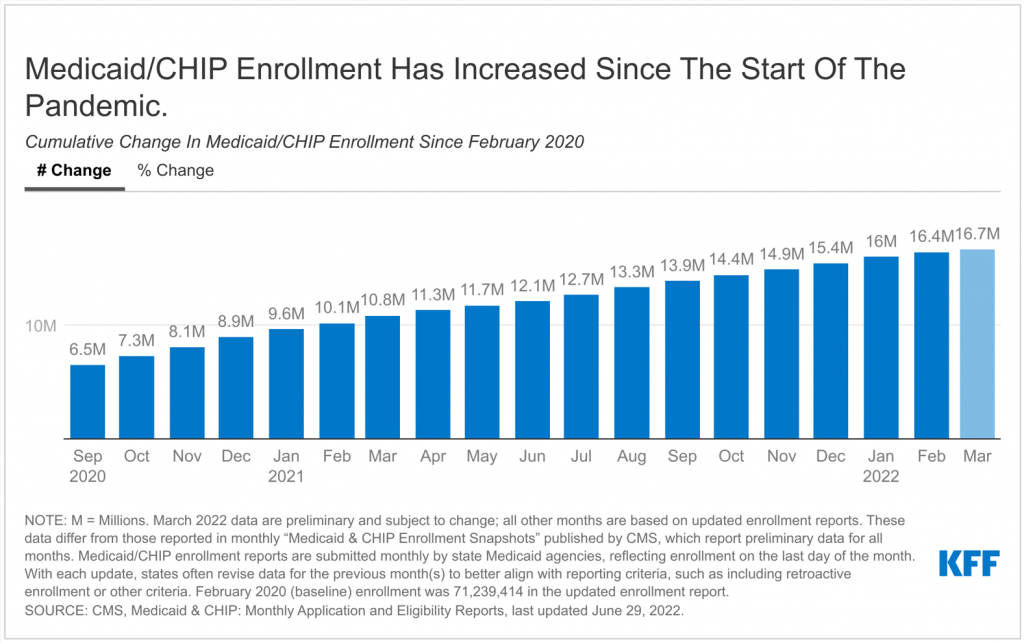
This data note looks at national and state-by-state Medicaid and CHIP enrollment data through March 2022. After declines in enrollment from 2017 through 2019, preliminary data for March 2022 show that total Medicaid/CHIP enrollment grew to 87.9 million, an increase of 16.7 million from enrollment in February 2020 (23.4%), right before the pandemic and when enrollment began to steadily increase (Figure 1). Increases in enrollment may reflect changes in the economy, changes in policy (like recent adoption of the Medicaid expansion in the Affordable Care Act), and the temporary continuous enrollment requirement created by the Families First Coronavirus Response Act (FFCRA). Under the continuous enrollment requirement, states generally cannot disenroll Medicaid enrollees during the emergency period and in exchange, states receive a temporary increase in the federal Medicaid match rates. The continuous enrollment requirement has halted churning in Medicaid – the temporary loss of coverage in which enrollees disenroll and then re-enroll within a short period of time – in addition to preventing Medicaid coverage loss during the public health emergency. While enrollment has increased for 25 consecutive months, the monthly increases appear to be slowing compared to early in the pandemic.
The information in this data note is based on KFF analysis of the Centers for Medicare and Medicaid Services (CMS) Performance Indicator Project Data. Medicaid/CHIP enrollment data are submitted monthly by state Medicaid agencies, and with each monthly update, states often revise the previous months’ enrollment to include retroactive enrollment and to better align with reporting criteria. Except for the latest month’s enrollment (March 2022), this brief reports data from the updated enrollment reports for all other months to reflect the most current enrollment data possible. However, the data presented in this brief will differ from those presented in monthly Medicaid and CHIP Enrollment Snapshots published by CMS, which use exclusively preliminary enrollment reports for all months.
Medicaid/CHIP enrollment increased following the implementation of the Affordable Care Act (ACA) but was declining in the two years prior to the pandemic. Following the implementation of the ACA Medicaid expansion to low-income adults in 2014, there were large increases in Medicaid and CHIP enrollment across states that followed steady growth in coverage of children over the past decade. These increases reflected enrollment among newly eligible adults in states that implemented the expansion as well as enrollment among previously eligible adults and children due to enhanced outreach and enrollment efforts and updated enrollment procedures tied to the ACA. This trend began reversing when enrollment started to decline in 2018 and continued to decline in 2019. Total enrollment fell from 73.4 million in December 2017 to 71.2 million in December 2019, a decline of 2.2 million people or 3.0%. Month-to-month enrollment declines slowed but continued until February 2020. The declines in enrollment, in part, reflected a robust economy, but experiences in some states suggested that they may have also reflected enrollment losses among people who were still eligible for coverage due to challenges completing enrollment or renewal processes.
Data show that Medicaid/CHIP enrollment is increasing amid the coronavirus pandemic, growing by 16.7 million enrollees or 23.4% from February 2020 to March 2022. Over this period, all states experienced total Medicaid/CHIP enrollment growth ranging from 14.9% to 64.5% (Figure 2). The state with the largest growth since February 2020, Oklahoma, implemented the Medicaid expansion on July 1, 2021. Four other states have implemented expansion since 2020 – Utah and Idaho in January 2020, Nebraska in October 2020, and Missouri (where the state began to process applications in October with coverage retroactive to 7/1/2021) – contributing to higher-than-average rates of enrollment growth in these states as well.
Virtually all growth was concentrated in Medicaid, which grew by 25.4% (16.4 million enrollees) from February 2020 to March 2022 data (Figure 3). Conversely, CHIP has seen very little enrollment growth since February 2020 (3.6% or 244,000 enrollees) and several states (16) have seen declines in CHIP enrollment from February 2020 through March 2022. These declines in CHIP enrollment for some states could reflect changes in family income, causing children to move from CHIP to Medicaid coverage. As discussed below, all states reported increases in child enrollment for Medicaid/CHIP overall during this time period.
Adult enrollment in Medicaid/CHIP has increased rapidly during the pandemic, growing by 32.3% from February 2020 through March 2022 (Figure 4). This growth amounts to an additional 11.1 million adults in the 49 states and DC that report adult/child monthly enrollment (Arizona does not report children or adults separately). As mentioned above, five states began newly enrolling expansion adults since January 2020 (Idaho, Missouri, Nebraska, Oklahoma, and Utah), contributing to increased adult enrollment. Child enrollment grew as well, but at a slower pace: 14.5% or 5.1 million enrollees in the same period. Still, every state reporting these data saw an increase in child Medicaid/CHIP enrollment from February 2020, despite declines in CHIP enrollment in some states (as discussed above).
When the continuous enrollment requirement expires, many could lose coverage as states resume more regular renewal processes. The continuous enrollment requirement will last until the end of the month in which with national public health emergency (PHE) ends. Currently, the PHE is in effect through mid-July 2022, although it is expected that the PHE will be extended for at least another three months (because the Biden administration did not provide a 60-day notice to states as of May). Until the PHE expires, Medicaid enrollment is likely to continue to grow at a slow pace. At the end of the continuous enrollment requirement, states will have up to 14 months to complete redeterminations and resume normal operations, although some states have indicated that they may complete redeterminations more quickly. During this time, states will begin disenrolling people who no longer qualify or who face administrative barriers, such as responding to mailed requests for information within a set timeframe, even though they may still be eligible. Recent KFF estimates indicate that between 5.3 million and 14.2 million Medicaid enrollees could be disenrolled in the months following the end of the continuous enrollment requirement. How states manage the large volume of redeterminations during the “unwinding” of the continuous enrollment requirement, as well as how states engage with enrollees and other stakeholders, will impact the continuity of coverage for millions of Medicaid enrollees.