Recent Trends in Mental Health and Substance Use Concerns Among Adolescents
Concerns about adolescent mental health and substance use have increased recently, particularly in light of gun violence and the COVID-19 pandemic. In recent years, many adolescents have experienced worsened emotional health, increased stress, and a lack of peer connection. Other mental health and substance use concerns are on the rise – including drug overdose deaths, self-harm, and eating disorders. Simultaneously, adolescents are spending more time on screens and many report adverse experiences such as parental abuse, hunger, and job loss – all of which can be linked to poor mental health outcomes.
This brief explores the state of adolescent mental health and substance use in recent years, highlighting differences observed by sex, racial and ethnic groups, and sexual orientation. Throughout this analysis, we define adolescents as individuals ages 12 to 17. Although data on adolescent mental health is limited, where possible, we draw upon data from the 2020 National Survey of Children’s Health (NSCH), which asks parents or guardians questions on behalf of their children and adolescents. We also include data from the Centers for Disease Control and Prevention (CDC) and other surveys conducted during the pandemic.
Key takeaways include:
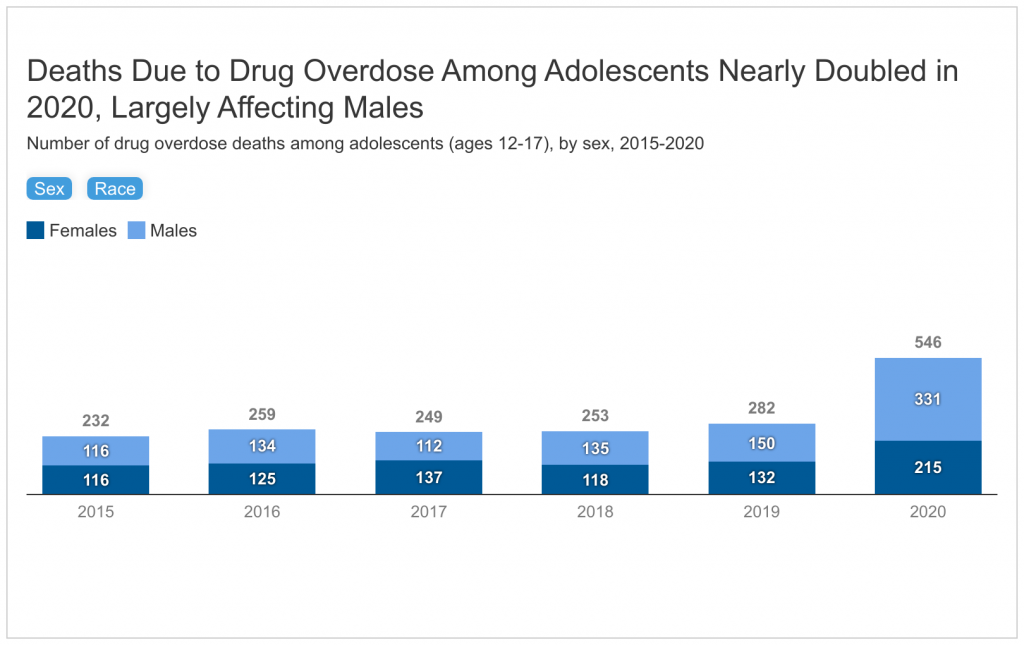
- Deaths due to drug overdose among adolescents nearly doubled from 2019 (282 deaths) to 2020 (546 deaths). In the same time period, the largest increases in these deaths were among adolescent males (deaths more than doubled), as well as Black (deaths more than tripled) and Hispanic (deaths more than doubled) adolescents.
- Suicides are the second leading cause of death among adolescents. These deaths have increased since 2010 but slowed in recent years. It is possible that not all suicides are captured as they may be misclassified as drug overdose deaths. In 2020, across racial and ethnic groups, suicide death rates were highest among American Indian and Alaska Native adolescents (22.7 per 100,000) followed by White adolescents (4.5 per 100,000). Adolescent males had higher rates of suicide compared to their female peers (8.7 vs. 3.9 per 100,000); however, rates of self-harm were higher (and increasing faster) for females.
- The share of adolescents experiencing anxiety and/or depression has increased by one-third since 2016 but held relatively steady from 2019 (15%) to 2020 (16%). In 2020, anxiety and/or depression was more pronounced among adolescent females than males. Anxiety and/or depression was higher among White and Hispanic adolescents and lower among Black adolescents.
- In 2021, many adolescents reported adverse experiences such as emotional abuse (55%), parental job loss (29%), hunger (24%), and physical abuse (11%). Some of these experiences were more pronounced among female and lesbian, gay, or bisexual (LGB) adolescents. Research shows that gun violence, including but not limited to school shootings, has continued to rise in recent years and may be linked to poor mental health outcomes among youth.
- Access to mental health care may have worsened during the pandemic with declines in utilization of care among both Medicaid and private insurance pediatric beneficiaries. Prior to the pandemic, receipt of mental health treatment was low and varied across demographics. Reasons for not receiving care included costs and a lack of providers.
Looking ahead, states, the Administration and Congress are taking actions and proposing new policies to address the national mental health crisis. Congress is also considering a package of mental health provisions in response to recent gun violence.
How have substance use and related deaths among adolescents changed in recent years?
Deaths due to drug overdose among adolescents nearly doubled in the first year of the pandemic, likely driven by illicit fentanyl. After remaining stable for several years, drug overdose deaths among adolescents increased from 282 deaths in 2019 to 546 deaths in 2020 (Figure 1). The rise in fentanyl-laced substances are likely the primary driver behind this change.
In the first year of the pandemic, drug overdose deaths more than doubled among adolescent males. After a period of relative stability, both males and females experienced large increases in drug overdose deaths from 2019 to 2020 (Figure 1). As a result of these increases, the gap in the rate of drug overdose deaths between adolescent males and females has widened from 2019 (1.2 per 100,000 males vs. 1.1 per 100,000 females) to 2020 (2.6 per 100,000 males vs. 1.7 per 100,000 females).
Drug overdose deaths have increased across all racial and ethnic groups, and particularly among Hispanic and Black adolescents. In the first year of the pandemic, the largest increases in drug overdose deaths were among adolescents of color (Figure 1). While White adolescents continue to account for the largest share of drug overdose deaths, adolescents of color are accounting for a growing share of these deaths over time. Between 2015 and 2020 the share of drug overdose deaths among White adolescents fell from 68% to 53%, while at the same time the shares of deaths among their Hispanic and Black peers rose (from 18% to 30% and 10% to 13%, respectively) (Figure 2). As a result of this increase, Hispanic adolescents now account for a disproportionate share of drug overdose deaths relative to their share of the total adolescent population (30% vs. 25%).
Although drug overdose deaths among adolescents increased from 2019 to 2020, the use of some other substances (e.g., alcohol and illicit drug use) has declined in the last decade. In 2021, nearly a third (32%) of high school students reported using alcohol, tobacco, or marijuana or misuse of prescription opioids. Substance use was more pronounced among several subpopulations, including LGB and American Indian and Alaska Native (AIAN) adolescents (Appendix Table 1). However, findings on whether substance use has increased among adolescents during the pandemic are mixed. Some research has shown that substance use decreased in 2021 among adolescents. Other research found that among high school students who used substances prior to the pandemic, nearly one in three reported increases in substance use in 2021. Leading up to the pandemic – from 2009 to 2019 – declines were seen in cigarette smoking (from 20% to 6%), alcohol use (from 42% to 29%), and illicit drug use (from 23% to 15%) among adolescents. During the same time period, substance use continued to vary across demographics, similar to patterns observed in 2021. Early initiation of substance use is associated with increased risk of addiction later in life.
How have suicide and self-harm among adolescents changed in recent years?
Among adolescents, deaths due to suicide increased from 2010 to 2018 and then slowed in 2019 and 2020. Suicide is the second leading cause of death among adolescents. From 2010 to 2020, the suicide death rate grew by 62% (Figure 3). These suicides increased from 2010 to 2018, declined in 2019, and remained relatively stable in 2020. It is possible that some suicides are misclassified as drug overdose deaths since it can be difficult to determine whether drug overdoses are intentional. Forty-four percent of adolescent suicides were by firearms in 2020, up from 38% in 2010.
Suicide death rates have increased across all racial and ethnic groups over time and remain highest among American Indian and Alaska Native adolescents. AIAN adolescents continue to have the highest suicide death rate compared to their peers and remain over three times as likely to die by suicide than White adolescents (22.7 vs. 7.3 per 100,000 in 2020) (Figure 3). In contrast, Black, Hispanic, and Asian adolescents had lower rates of suicide deaths compared to their White peers, but they experienced larger increases in suicide death rates over time. These death rates more than doubled for Asian adolescents (from 2.2 to 5.0 per 100,000 from 2010 to 2020) and nearly doubled for Black (from 2.4 to 4.6 per 100,000 from 2010 to 2020) and Hispanic adolescents (from 2.8 to 5.0 per 100,000 from 2010 to 2020). Beginning in 2018, suicide death rates began to slightly decline among White and Asian adolescents but remained stable among Black and Hispanic adolescents.
Among adolescents, males and those living in non-metropolitan areas experienced much higher suicide rates than their respective peers. Differences in deaths by suicide also persist by sex and location. Although there has been a slight decline in suicide death rates among adolescent males since 2018, these rates remain much higher than death rates for their female peers (8.7 vs. 3.9 per 100,000 in 2020) (Figure 3). Since 2010, suicide death rates among adolescents in metropolitan areas have increased faster than among adolescents in non-metropolitan areas. However, adolescents in metropolitan areas consistently have a lower suicide death rate than their peers (5.9 vs. 8.8 per 100,000 in 2020).
Despite stable suicide rates among adolescents in 2020, self-harm and suicide attempts have increased, particularly among females. The rate of emergency department visits for self-harm (defined as self-injury or poisoning with the intent to harm oneself or take one’s own life) increased by 10% among adolescent females from 2019 to 2020 (from 657 to 724 per 100,000). These rates, however, remained stable among adolescent males (192 to 195 per 100,000 from 2019 to 2020) and significantly lower than their female peers (Figure 4). Although the rate of self-harm was nearly four times higher among adolescent females than males in 2020, the rate of deaths by suicide was twice as high among adolescent males compared to females in the same year. Other analyses found that as the pandemic progressed, emergency department visits for suicide attempts increased among adolescents, primarily driven by females.
How have anxiety and depression among adolescents changed in recent years?
The share of adolescents experiencing anxiety and/or depression has increased over time but remained relatively stable in the first year of the pandemic. Sixteen percent of adolescents experienced anxiety and/or depression in 2020 (16%) which is similar to the share in 2019 (15%), but significantly higher than in 2016 (12%) (Figure 5). Anxiety and depression can co-occur with other mental health disorders and are associated with suicide and substance use.
Anxiety and depression are more pronounced among adolescent females and White and Hispanic adolescents. The share of both adolescent females and males experiencing anxiety and/or depression has increased over time but remains higher among females compared to males (18% vs. 14% in 2020) (Figure 5). White and Hispanic adolescents have also seen increases in anxiety and/or depression over time although the rate has remained stable among Black adolescents (Figure 5). From 2016 to 2018, the share of Hispanic adolescents reporting anxiety and/or depression was lower than their White peers; however, in 2019 and 2020, the shares were statistically similar between these groups. Compared to their White peers, Black adolescents have been consistently less likely to report anxiety and/or depression over time. This finding may reflect underdiagnosis of mental health issues among children and adolescents of color due to gaps in culturally sensitive mental health care, structural barriers, and stigma associated with accessing care. Anxiety and/or depression data was not available for other racial and ethnic groups or by sexual orientation. However, a separate survey of high school students in 2021 found that lesbian, gay, or bisexual (LGB) students and students with another sexual identity other than heterosexual or students who were questioning their sexual identity were more likely to report persistent feelings of sadness and hopelessness than their heterosexual peers (76% and 69%, respectively vs. 37%). Similar differences between LGB and heterosexual high school students reporting persistent feelings of sadness and hopelessness were also found in a survey prior to the pandemic (66% vs. 37% in 2019). These feelings of sadness and hopelessness can be indicative of depressive disorder.
Eating disorders, which commonly co-occur with anxiety, have increased during the pandemic, particularly among adolescent females. Analyses of emergency department visits and hospital admissions during the pandemic found that, compared to prior to the pandemic, presentation of eating disorders increased sharply for adolescent females. Historically, eating disorders affect females more than males. These disorders can result in death.
What experiences among adolescents may negatively impact their mental health and well-being?
In 2021, many high school students reported adverse experiences, particularly female and LGB students. Large shares of adolescents reported experiences of parental emotional (55%) and physical abuse (11%), parental job loss (29%), and hunger (24%) in 2021. Some of these experiences were more pronounced among female and LGB adolescents. For example, reported parental emotional abuse was higher among female high school students than males (63% vs. 47%), and higher among LGB high school students than their heterosexual peers (74% vs. 50%) (Appendix Table 2). Experiences such as abuse and financial and food insecurities can lead to significant stress among children and may impact their cognitive abilities and increase the risk of suicide. Social supports, including relationships with peers, can be a protective factor among adolescents in the face of adverse experiences. In 2021, however, peer connections were strained – only 47% of high school students reported feeling close to people at school.
Gun violence continues to rise and may lead to negative mental health impacts among children and adolescents. An increasing number of children and adolescents have been exposed to gun violence in recent years. There were 42 school shootings across the U.S. in 2021 – the highest on record for a single year – and in 2020 firearms became the leading cause of death among children ages 19 and below. Research suggests that children and adolescents may experience negative mental health impacts, including symptoms of anxiety, in response to school shootings and gun-related deaths in their communities. Other research found that youth antidepressant use increased following exposures to fatal school shootings.
How has the pandemic affected access to care?
Leading up to the pandemic, access to mental health care varied across demographics. Adolescent males and adolescents in rural areas were less likely than their respective counterparts to access care. Compared to their White peers, children of color were also less likely to access care. In general, receipt of mental health treatment was low prior to the pandemic, with only one in five children and adolescents with mental, emotional, or behavioral disorders receiving mental health care from a specialized provider. Reasons for not receiving mental health care included costs, limited insurance coverage, social stigma, confidentiality concerns, a lack of providers, and the absence of culturally competent care.
During the pandemic, access and utilization of mental health care may have worsened. Among Medicaid and CHIP beneficiaries, utilization of mental health services declined by 23% for beneficiaries 18 and younger from March 2020 to August 2021 compared to prior to the pandemic; and utilization of substance use disorder services declined by 24% for beneficiaries ages 15-18 for the same time period. Private mental health care claims decreased from 2019 to 2020 among adolescents age 13-18. Despite a drop in the total number of mental health claims among privately insured patients, mental health care represented a larger share of total medical claims among these patients in 2020 than in 2019. Additionally, many children ages 18 and younger began accessing mental health and substance use care through telemedicine in light of the pandemic. However, as the pandemic continued into 2021, outpatient care through telemedicine began to decline among children. Separately, anecdotal evidence also suggests that the availability of inpatient psychiatric services has decreased during the pandemic, impacting children in need of emergency care during a mental health crisis.
What to watch?
Several measures have been taken or proposed to address worsening mental health and barriers to care. The U.S. Preventive Services Task Force has put forth draft recommendations to screen adolescents ages 12 to 18 for major depressive disorder and children ages 8 to 18 for anxiety. Additionally, many state Medicaid programs plan to implement new crisis services and have already expanded coverage of telemedicine services for mental health and substance use care. In July 2022, 988 – a federally mandated crisis number – will launch, providing a single three-digit number for individuals in need to access local and state funded crisis centers. The Biden Administration released a strategy to address the national mental health crisis in May 2022, building on prior actions. There have also been bipartisan bills introduced that would designate funding towards the integration of behavioral health care into pediatric primary care, youth suicide prevention, and support for individuals with eating disorders. A separate bipartisan bill supporting mental health and suicide prevention services in schools was also introduced. Most recently, in response to gun violence, the Bipartisan Safer Communities Act was signed into law and allocates funds towards mental health, including trauma care for school children. A large share of the American public (42%) report that increasing government funding for access to mental health services and training for mental health providers should be a top priority for Congress, though a number of other health care issues rank higher.
Despite recent attention and responses, challenges remain in addressing worsening adolescent mental health and access to care issues. Mental health and substance use issues among adolescents have increased over time and remain more pronounced among several subgroups. Some states have recently considered policies that would limit LGBTQ+ youth access to gender affirming care, which, if enacted, may further contribute to poor mental health among this population. Additionally, gun violence and active shooter drills in schools may further contribute to poor mental health outcomes among youth. If left untreated, mental health conditions that develop during adolescence can persist into adulthood and limit quality of life. Looking ahead, data on vulnerable populations will be pivotal in further understanding how to address and mitigate rising mental health and substance use concerns.
If you or someone you know is considering suicide, contact the National Suicide Prevention Lifeline at 1-800-273-8255 (For Spanish: 1-888-628-9454; Deaf and Hard of Hearing: 1-800-799-4889). Beginning July 16, 2022, you can dial 988 from any landline or cell phone to access crisis services.
This work was supported in part by Well Being Trust. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
Elizabeth Williams, Policy Analyst at KFF, provided analysis of 2016-2020 National Survey of Children’s Health data.
Appendix